What Does Pnp Stand For Sexually
👉🏻👉🏻👉🏻 ALL INFORMATION CLICK HERE 👈🏻👈🏻👈🏻
"Party and Play" ... "party" means drugs, often meth (crystal/tina) or E, "play" means sex. Usually leads to long, chemmed-up sex sessions. Usually seen in chat room or ads.
SWM, 28, 6'2", 185#, 43c,32w, 8 cut, looking for some PnP with some nasty chicks
a spanish word meaning the flipflop
used by latin moms to beat their child's ass
Latin mom: DO U NOT FUCKING LISTEN CHILD
Latin child: OH SHIT NOT LA CHANCLA
Get the la chancla neck gaiter and mug.
Seen most often in the gay community, slang for Party n' Play. Party refers to drug use- most often meth (tina, ice, crank) but sometimes ecstasy (E, XTC, Adam) cocaine (coke, blow, ski, snow), or poppers as well(though the latter is not generally considered a PnP item. Play refers to sex. PnP is considered a scene in itself- sex and drugs.
U into PnP?
Na, man, I don't touch that shit.
Get a PnP mug for your sister Sarah.
Abbreviation of the words "Party and Play" - a phrase used to refer to the act of taking illicit substances prior to or during sexual intercourse. The term is most commonly used amongst gay men to refer to recreational use of club/party drugs in the context of "chemsex".
A: "What are you into?"
B: " Versatile top here. Into Bb, fetish, group, pnp"
Get a PNP mug for your cousin Paul.
(pee-en-PEE) verb. abbreviation for party and play as relating to homosexual men engaging in sexual acts while high on methamphatimine (see p and p and crystal dick)
Tod: "Hey Tim. What are you doing this weekend?"
Tim: "I was invited to Tad's."
Tod: "Oh, that's right! Ted told me he got a teener.
Tim: "Yeah! Now I'll get laid."
Tod: "So, you guys are gonna p n' p huh?"
Tim: "I hope so."
Get the p n' p neck gaiter and mug.
Acronym for "Party N Play." Party means smoke or inject crystal methamphetamine (speed) into your system. N Play refers to the marathon sex that follows after you're all jacked up on speed and want to "Play" all night.
Looking to PNP with Tina. Looking for guys who want to PNP with me all night. Looking to PNP and have WILD sex.
Get a PNP mug for your sister Nathalie.
Used in chat rooms as the adreviation for "Party and Play". To meet have sex and alcohol or other drug.
Get a PnP mug for your brother Georges.
To read the full-text of this research, you can request a copy directly from the author.
To read the full-text of this research, you can request a copy directly from the author.
Sexual abuse is a problem of epidemic proportions in the United States. In their practice, pediatric nurse practitioners will likely encounter children who have experienced sexual abuse—both those who have and have not previously been identified as victims. Sexually transmitted infections (STIs) are rare in sexually abused children and adolescents. However, when present, they can be crucial to making the diagnosis of sexual abuse and protecting children. This continuing education article will assist the pediatric nurse practitioner in interpreting the relationship between STIs and sexual abuse, correctly testing for STIs, and treating STIs in children and adolescents.
To read the full-text of this research,
you can request a copy directly from the author.
... Hepatitis B is a serious and major public health problem despite the presence of an effective vaccine. 1 The hepatitis B virus (HBV) is a well-known blood-borne virus because it is transmitted through exposure to infective blood, semen, and other body fluids, peripheral blood mononuclear cells (PBMCs) and sharing needles. 2 Acute HBV can be a self-limiting or it can be chronic infection and increases the risk of developing liver failure, Hepatocellular carcinoma (HCC) or cirrhosis. 3 HBV infection is a major cause of chronic liver disease, affecting more than 240 million people worldwide. ...
Hepatitis B virus is a major public health impasse all over the world. Recently a new form of hepatitis B infection named Occult hepatitis B Infection (OBI) has appeared globally. The OBI is defined as the presence of HBV DNA in the liver and/or blood in the absence of detectable serum HBsAg with/without anti-HBc or anti-HBs. The prevalence of OBI has been reported in hemodialysis (HD) patients in different regions of the world. Thus, this study investigated the prevalence of OBI among HD patients. The cross-sectional study was carried out on 84 HD patients. These sera were checked for HBsAg, HBc-IgG assessment using Enzyme linked immunosorbent assay. The DNA was extracted from the sera samples and tested for HBVDNA detection using Nested Polymerase Chain Reaction (Nested PCR). The liver function tests including serum alanine aminotransferase and aspartate aminotransferase levels were carried out for all the HD individuals. 52/84(61.9%) of HD were males and 32/84 (38.1%) were females. The patient’s age ranged from 25 to 64 with a mean age of 52.4±15.2 years. HBsAg and HBc-IgG were detected in 1(1.1%) female. 2 (2.4%; a female and a male) patients were positive for HBsAg. 14/84 (16.7%; 6 female and 8 male) HD patients were positive for anti-HBc but negative for HBsAg, among them 4(28.6%; 2 female and 2 male) cases were positive for HBV DNA, indicating the presence of OBI in HD patients. Even distribution of OBI among the HD was found in 2(2.36%) male and 2(2.36%) female (P>.0.05). In the present study the moderate rate of 4.76% OBI has been observed in HD patients. The prevalence of seropositive OBI among the gender was 2(2.36%) male and 2(2.36%) female. The seronegative OBI have not been detected in the present study but requires further investigation. In this study the affliction of OBI in HD patients is not clear.
... 109 Factors that may indicate need for sexually transmitted infection testing include child disclosure of contact sexual abuse, genital and/or anal discharge, unexplained genital and/or anal injury, and known or suspected contact with infected perpetrator. 126 If untrained in this evaluation, clinicians need to know how to respond to suspected CSA by reporting the case to CPS and referring the child for evaluation by another medical professional with appropriate expertise. 109 Pediatric clinicians play a vital role in the identification and treatment of suspected child sexual abuse. ...
Neonatal infection with Trichomonas vaginalis is an unusual occurrence. We present a case of T. vaginalis found on routine urinalysis in a five-day-old neonate born at 29 weeks gestational age. The patient was treated with metronidazole and had complete resolution of the infection. This report discusses the significance of diagnosis and treatment of T. vaginalis in the neonate.
Sexual abuse is unfortunately common in the United States. The presence of a sexually transmitted infection in a child or adolescent should prompt an evaluation to exclude sexual abuse. The present article reviews the demographics of sexual abuse, the prevalence of specific sexually transmitted infections, such as Neisseria gonorrhoeae, Chlamydia trachomatis, HIV, human papillomavirus (HPV) and herpes simplex virus (HSV) and which children and adolescents are at highest risk for contracting such infections. The use of nonculture methods, such as nucleic acid amplification tests (NAATs), to evaluate prepubertal children for N. gonorrhoeae or C. trachomatis, and the use of HIV postexposure prophylaxis are discussed. Any child or adolescent with a sexually transmitted infection should be evaluated for sexual abuse. Specific infections in prepubertal children, such as Neisseria gonorrhoeae or Chlamydia trachomatis, are due to abusive contact and should be reported to Child Protective Services. As the modes of transmission of anogenital infections with HPV and HSV are unclear, an evaluation for sexual abuse should be done. Although transmission of HIV after sexual abuse is rare, HIV postexposure prophylaxis must be administered in a timely fashion, and adequate outpatient support provided to facilitate compliance and follow-up.
Purpose of review: Eastern Europe and Central Asia (EECA) has experienced large-scale epidemics of syphilis, hepatitis C virus (HCV) and HIV over the past few decades. Here, we review recent evidence on the epidemiology of and the response to these intersecting epidemics. Recent findings: The HIV epidemic in EECA continues to expand, with new infections increasing by more than 50% between 2010 and 2015. HCV is now in the top 10 causes of death in EECA, with Russia accounting for more than half of the global burden of HCV infections, but access to direct-acting antivirals remains a major obstacle for control of the epidemic. Although syphilis incidence is generally declining, high prevalence is reported in key populations, particularly sex workers and people who inject drugs. Recent epidemiological studies have highlighted very high prevalence of HIV, syphilis and HCV in prison populations, alongside poor access to prevention and treatment. Summary: Multiple factors are contributing to the ongoing and overlapping HIV, HCV and syphilis epidemics in EECA, including low coverage with antiretroviral therapy and insufficient scale of prevention services. Further research is required to estimate the burden of infections and identify effective prevention and treatment strategies in hard-to-reach key populations, particularly men who have sex with men.
The presence of sexually transmitted infections (STIs) in patients with suspected sexual abuse is uncommon in the field of pediatrics. To establish the prevalence of anogenital findings and their relation to the presence of STIs in girls referred for suspected child sexual abuse. Retrospective study conducted between January 1st, 2003 and December 31st, 2013. Physical findings and detection of STIs in girls with suspected child sexual abuse were analyzed. One thousand thirty-four patients were included. Their median age was 7.9 years old. Anogenital findings were classified as class I (normal):38.4%, class II (nonspecific):38.1%, class III (specific):19.9% and class IV (definitive):3.6%. STIs were observed in 42 patients (4.1%). A relation was established between STIs and the classification of physical findings: 10 (class II: 9; class III: 1) Neisseria gonorrhoeae, 17 (class I: 2; class II: 8; class III: 7) Chlamydia trachomatis, 15 (class I: 2; class II: 10; class III: 3) Trichomonas vaginalis. Statistically significant differences for Trichomonas vaginalis (p= 0.01) and Neisseria gonorrhoeae (p < 0.0001) were observed, with predominance of nonspecific clinical signs. Both nonspecific and specific findings were similarly observed for Chlamydia trachomatis (p= 0.03). Most cases of girls with suspected child sexual abuse had normal or nonspecific anogenital findings. The prevalence of STIs in these girls is low. Trichomonas vaginalis and Neisseria gonorrhoeae were related to nonspecific findings, while both nonspecific and specific findings were observed for Chlamydia trachomatis.
The diagnosis of gonorrhea and/or chlamydia in a pre-pubertal children beyond the neonatal period is confirmatory of mucosal contact with infective bodily secretions and therefore highly concerning for sexual abuse. When such a diagnosis is made, a report to protective authorities is warranted so that safety and potential criminal activity may be evaluated concurrent with the medical management. Occasionally, despite perceived adequate medical management and protective safety plans, a child may present with a repeat positive result for sexually transmitted infections. In this scenario it is important for medical providers to carefully consider and be aware of the possible reasons for the repeat positive result which include: 1) treatment failure; 2) a new infection from repeated abuse; or 3) a falsely positive result due to the limitations of non-culture testing. . Pre-pubertal sisters were diagnosed with gonorrhea and chlamydia, treated with antibiotics, and the individual identified as having sexually abused them was removed from the home. Over a four month period, both continued to have positive testing for chlamydia via Nucleic Acid Amplification Test (NAAT) and/or culture. Concurrent to utilizing alternate antibiotic treatment options, protective authorities were alerted to the fact that this was likely a re-infection. The investigative team later determined that a second adult, who tested positive for gonorrhea and chlamydia, was also sexually abusing both girls. Disclosures of abuse regarding both adult individuals were deemed credible by authorities and supported with collateral information.
Condyloma acuminata are caused by human papilloma virus (HPV) 6 and 11 and most commonly present in the anogenital region. Most transmission among adults is via sexual transmission, but HPV and resulting anogenital warts in pediatric populations may be a result of perinatal vertical transmission, indirect transmission through contaminated objects or surfaces, autoinoculation, or sexual transmission. A 9-year-old premenarchal female presented with multiple perianal warts. She had no significant medical history, and denied history of any sexual contact, including sexual abuse. The external examination revealed multiple warts in the perianal region, but no lesions, discharge, inflammation, or external signs of trauma were visible. Tests for sexually transmitted infections were all negative. The warts were diagnosed as condyloma acuminata, and were subsequently treated with trichloroacetic acid 80% (TCA) in the provider's office. TCA was applied on 3 separate occasions 2 weeks apart, showing marked improvement at each visit. While both sexual and nonsexual means of transmission are possible, sexual abuse must always be considered in pediatric cases. It is recommended that investigators proceed delicately, because the investigation can be psychologically damaging for patients and their families. Treatment methods are a unique consideration for pediatric patients, as most options are painful and require multiple office visits. The benefits of self-administration at home must be weighed with the likelihood of patient compliance and need for ongoing evaluation by the provider.
The Centers for Disease Control and Prevention recommends nucleic acid amplification testing for chlamydia and gonorrhea in sexually abused girls. No studies describe performance of APTIMA Combo 2 Assay with second target confirmation on the same testing platform. This nucleic acid amplification testing is evaluated within a large child advocacy center. Girls 3 to 18 years, 35% of whom reported consensual sexual activity, were prospectively tested by APTIMA Combo 2 on urine/vaginal swabs and by vaginal culture. A case of infection was defined as positive culture or positive urine or vaginal swab nucleic acid amplification testing with second target confirmation. Sensitivity of APTIMA Combo 2 on urine was found to be superior to vaginal culture and comparable to APTIMA Combo 2 on vaginal swabs for both infections. APTIMA Combo 2 on urine is less invasive, and its use may be preferred in this traumatized population.
Children may acquire syphilis as a consequence of nonsexual close contact if family members or caregivers are infected by active syphilis. We described 3 cases of acquired secondary syphilis in Chinese preschool children who contracted the disease from their caregivers to draw attention to the potential for syphilis patients to transmit Treponema pallidum to the children they are caretakers for.
Neisseria gonorrhoeae infection in a prepubertal child is virtually diagnostic of sexual abuse, provided perinatal infection has been excluded. Therefore, it is imperative that Neisseria gonorrhoeae be correctly identified. We present two cases of false positive Neisseria gonorrhoeae meningitis encountered at two different children's hospitals. Both cases were evaluated by the child protection teams prior to establishing the correct diagnosis.
The American Academy of Pediatrics recommends that site-specific cultures be obtained, when indicated, for sexually victimized children. Nucleic acid amplification testing is a highly sensitive and specific methodology for identifying sexually transmitted infections. Nucleic acid amplification tests are also less invasive than culture, and this may provide an efficacious alternative for children suspected of being sexually abused.
Sexual abuse is a problem of epidemic proportions. Pediatric nurse practitioners (PNPs) will most likely encounter sexually abused children in their practice, both those who have been previously diagnosed and others who are undiagnosed and require identification by the PNP. This continuing education article will discuss the medical evaluation of children with concerns of suspected sexual abuse. Acute and non-acute sexual abuse/assault examinations will be discussed. Physical findings and sexually transmitted infections concerning for sexual abuse/assault will also be discussed.
Diagnosis of sexually transmitted infections in children suspected of sexual abuse is challenging due to the medico-legal implications of test results. Currently, the forensic standard for diagnosis of Chlamydia trachomatis (CT) and Neisseria gonorrhoeae (NG) infections is culture. In adults, nucleic acid amplification tests (NAATs) are superior to culture for CT, but these tests have been insufficiently evaluated in pediatric populations for forensic purposes. We evaluated the use of NAATs, using urine and genital swabs versus culture for diagnosis of CT and NG in children evaluated for sexual abuse in 4 US cities. Urine and a genital swab were collected for CT and NG NAATs along with routine cultures. NAAT positives were confirmed by PCR, using an alternate target. Prevalence of infection among 485 female children were 2.7% for CT and 3.3% for NG by NAAT. The sensitivity of urine NAATs for CT and NG relative to vaginal culture was 100%. Eight participants with CT-positive and 4 with NG-positive NAATs had negative culture results (P = 0.018 for CT urine NAATs vs. culture). There were 24 of 485 (4.9%) female participants with a positive NAAT for CT or NG or both versus 16 of 485 (3.3%) with a positive culture for either, resulting in a 33% increase in children with a positive diagnosis. These results suggest that NAATs on urine, with confirmation, are adequate for use as a new forensic standard for diagnosis of CT and NG in children suspected of sexual abuse. Urine NAATs offer a clear advantage over culture in sensitivity and are less invasive than swabs, reducing patient trauma and discomfort.
This study assessed the situational and sociodemographic characteristics of children infected with human immunodeficiency virus (HIV) from pediatric sexual abuse. A letter of inquiry was sent to 2147 professionals across health and social service disciplines involved with child abuse assessment, treatment, and prevention. Respondents working in programs where HIV antibody testing of abuse victims occurs and who had identified HIV infection in one or more abused children were sent a survey to assess the demographics of victims, the family/living situation where abuse occurred, alternative risks for HIV infection, bases for diagnosis of sexual abuse and for HIV antibody testing, and profiles of the perpetrator and type of abuse. Of 5622 estimated HIV antibody tests conducted during 113,198 sex abuse assessments, 28 children were infected with HIV and lacked any alternative transmission route to that of sexual abuse. A total of 41 HIV-infected children with a history of sexual abuse were identified. Thirteen cases had alternative risk factors and were excluded from analysis. Sixty-four percent of the 28 victims with sexual abuse as the sole risk factor were female and 71% were African-American. The mean age was 9 years. Coinfection with another sexually transmitted disease (STD) occurred in 9 (33%) cases. Sexual abuse was diagnosed on the basis of a victim disclosure in 21 (75%) cases. The basis for
What does pnp mean sexually? - Answers
Urban Dictionary: PnP
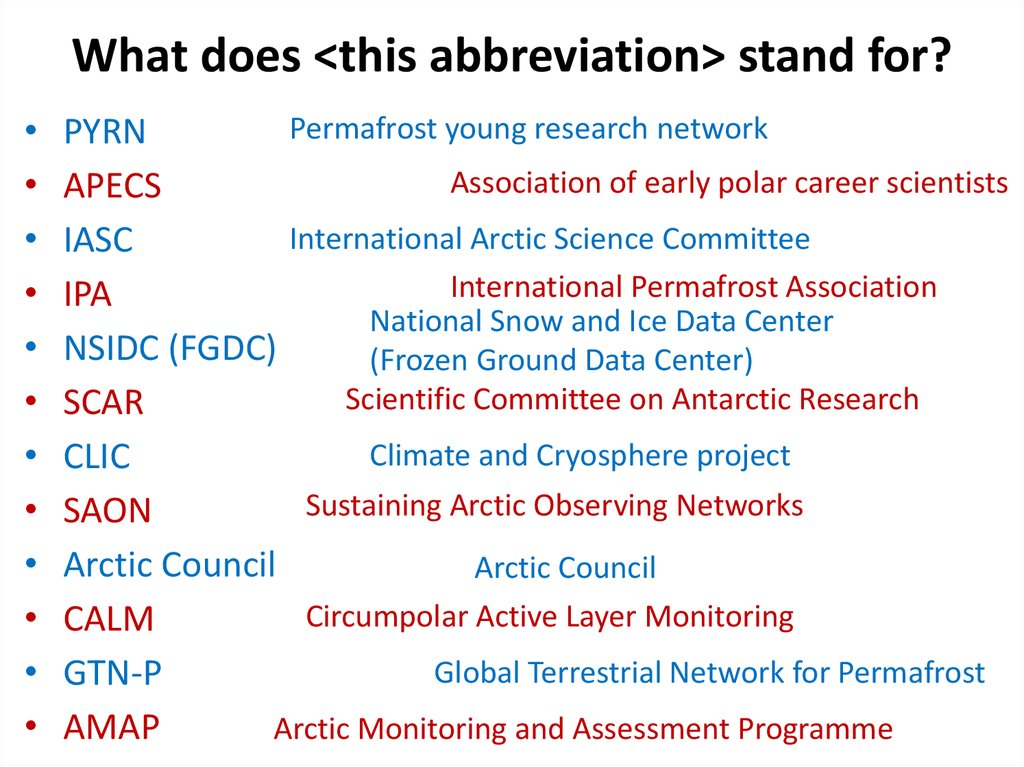
Sexually Transmitted Infections and Children: What the PNP Should Know
PNP - What Does PNP Abbreviation Mean?
Pansexual | LGBTA Wiki | Fandom
Japanese Teen Anal Tube
Betty_Boop
Japanese Nude Amateurs
What Does Pnp Stand For Sexually