Vaginal Prolapse

🛑 👉🏻👉🏻👉🏻 INFORMATION AVAILABLE CLICK HERE👈🏻👈🏻👈🏻
Call for Additional Assistance
800.223.2273
Vaginal prolapse is a condition where the vagina slips out of position. This is more common in women who have had multiple vaginal deliveries during childbirth, have gone through menopause, are smokers or are overweight. The chances of developing a prolapse also increases as you age.
Get useful, helpful and relevant health + wellness information
The Glickman Urological & Kidney Institute offers innovative treatments in urology and nephrology, including minimally invasive, scarless options for urologic procedures and medical management of kidney disease.
Cleveland Clinic’s Ob/Gyn & Women’s Health Institute is committed to providing world-class care for women of all ages. We offer women's health services, obstetrics and gynecology throughout Northeast Ohio and beyond. Whether patients are referred to us or already have a Cleveland Clinic ob/gyn, we work closely with them to offer treatment recommendations and follow-up care to help you receive the best outcome.
9500 Euclid Avenue, Cleveland, Ohio 44195 | 800.223.2273 | © 2021 Cleveland Clinic. All Rights Reserved.
Now scheduling COVID-19 vaccines for ages 12+ and third doses for eligible patients
Schedule your appointment
COVID-19 vaccine FAQs
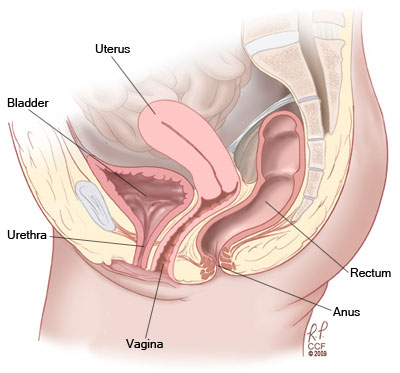
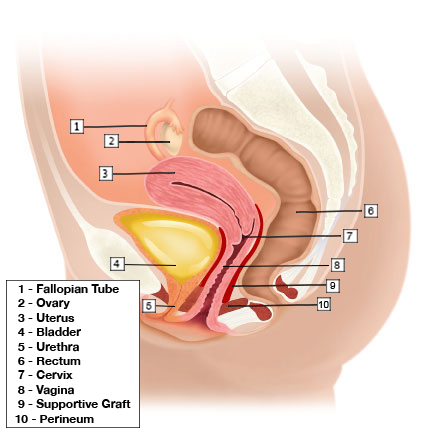
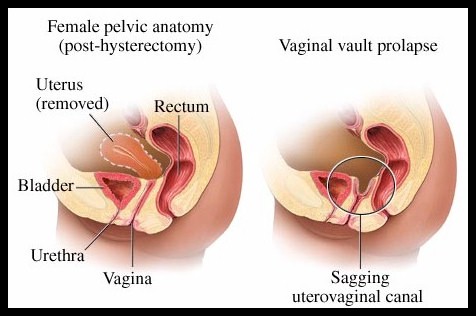
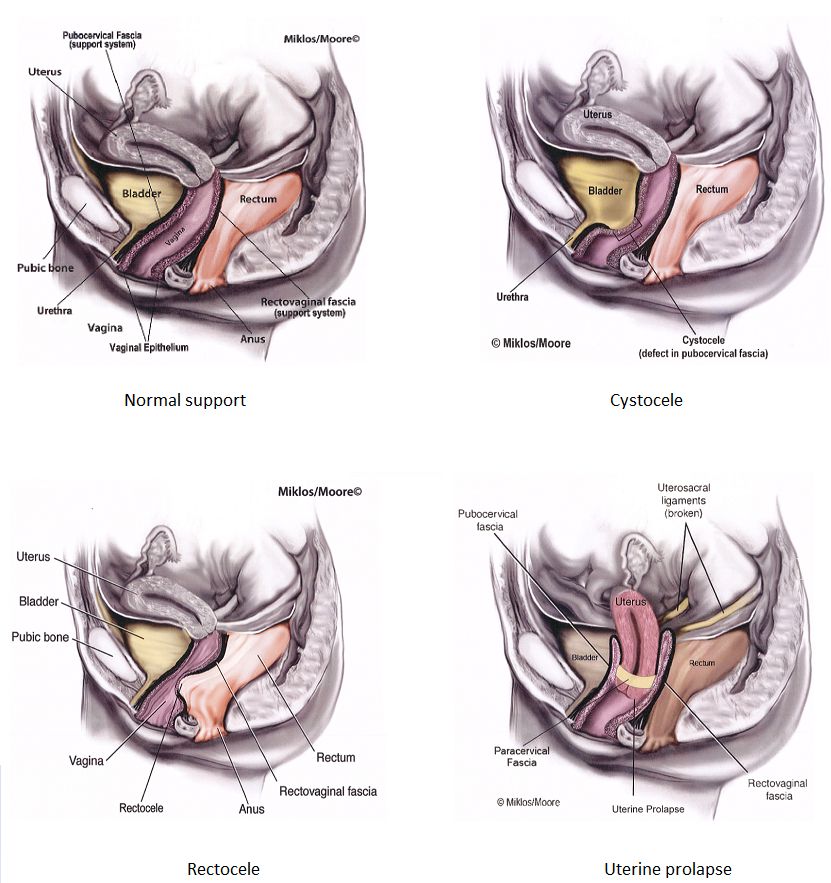
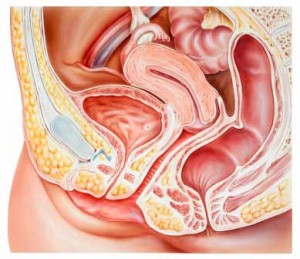
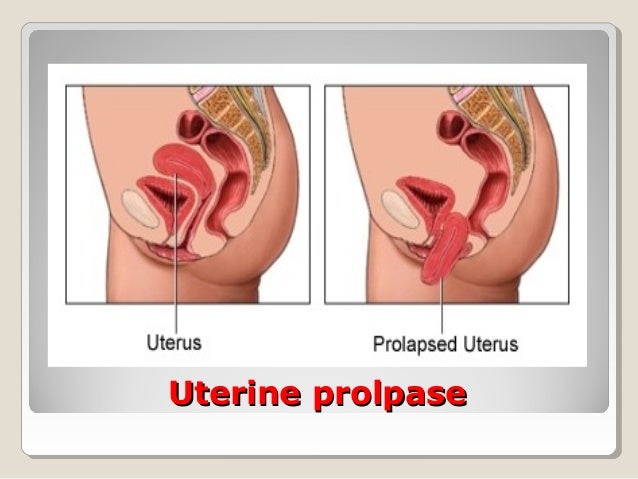
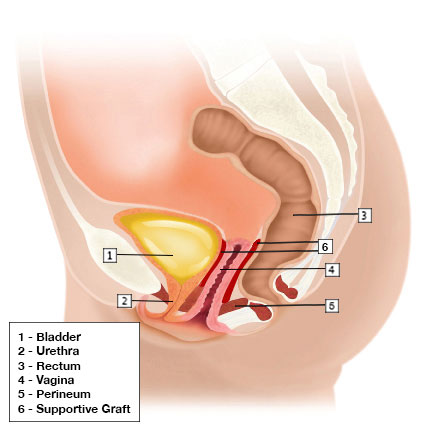
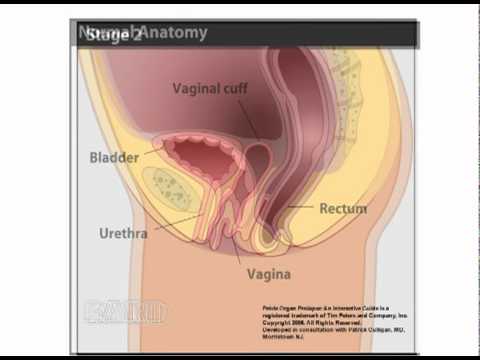
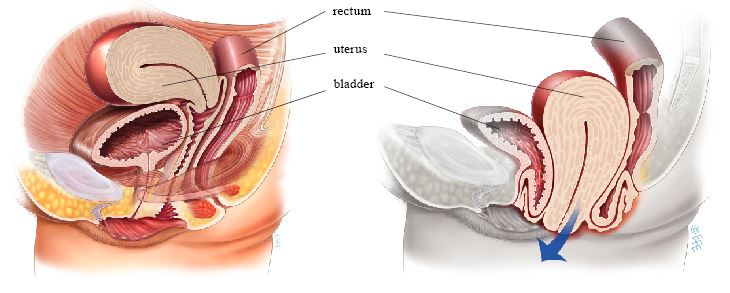
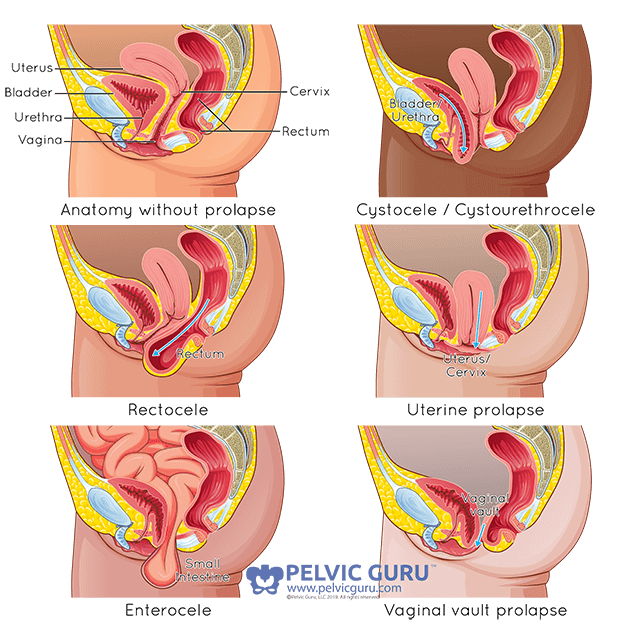
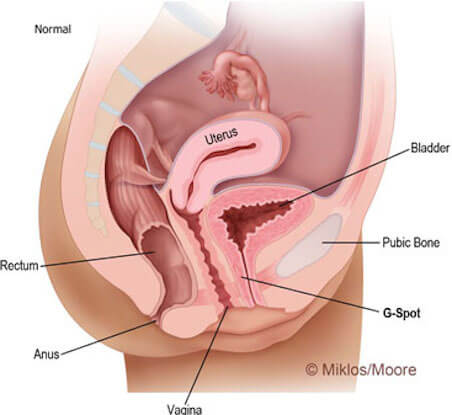
A vaginal prolapse is a dropping of your vagina from its normal location in the body. The vagina, also called the birth canal, is the tunnel that connects the uterus to the outside of a woman’s body. Your vagina is one of several organs that rests in the pelvic area of your body. These organs are held in place by muscles and other tissue. These muscles come together to create a support structure. Throughout your life, this support structure can start to weaken. This can happen for a variety of reasons, but the result is a sagging of your organs. When your organs sag or droop out of their normal position, this is called a prolapse.
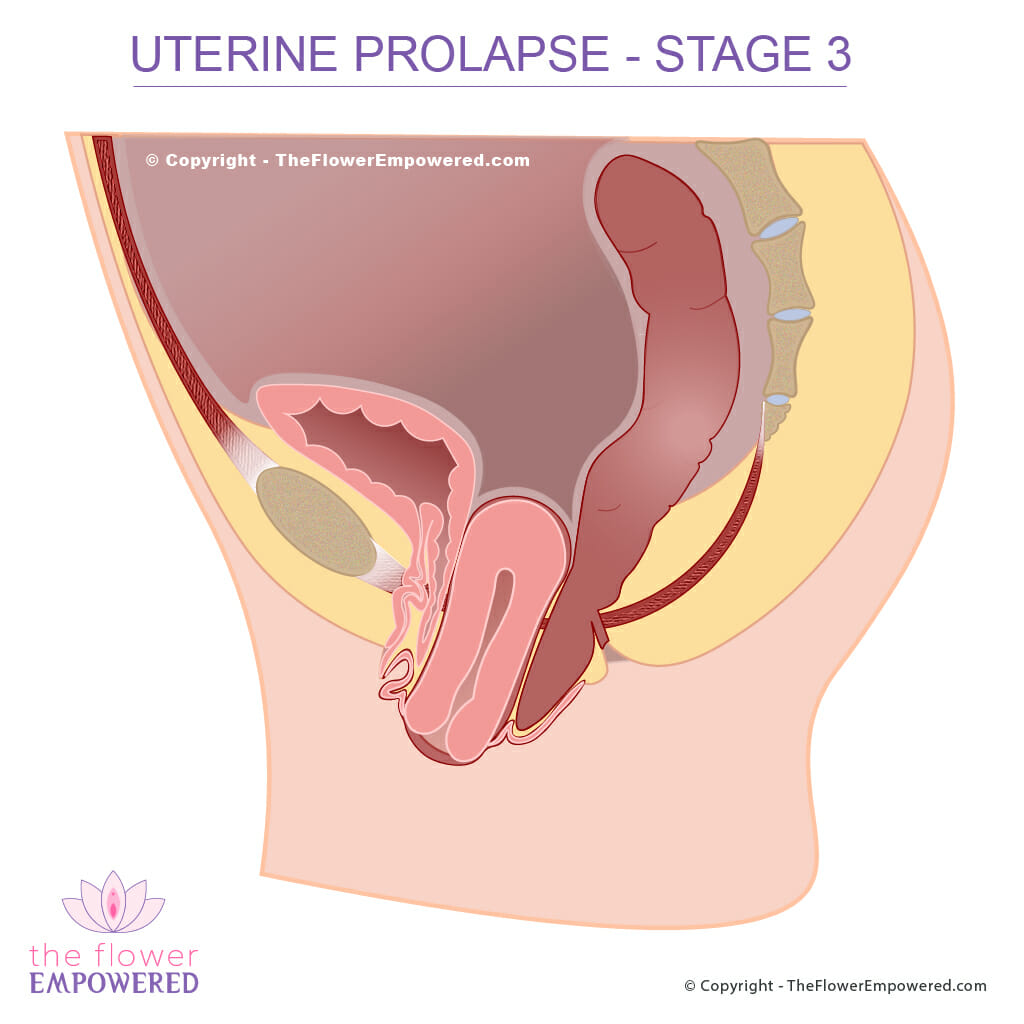
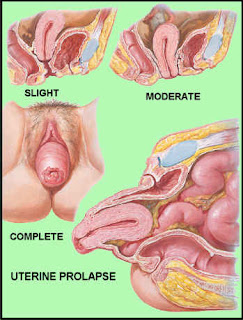
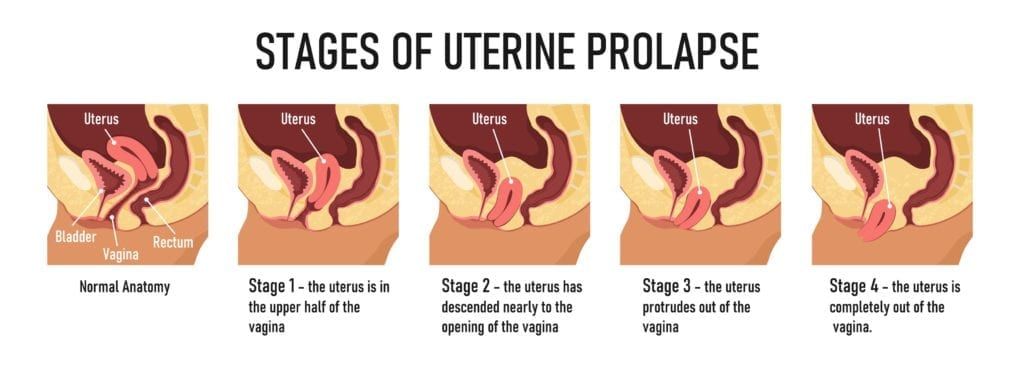
Prolapses can be small—with just a little movement—or large. A small prolapse is called an incomplete prolapse. A bigger prolapse (called a complete prolapse) is one where the organ has shifted significantly out of its normal place. A complete prolapse can result in part of the organ sticking out of the body. This is a very severe prolapse.
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services.
Policy
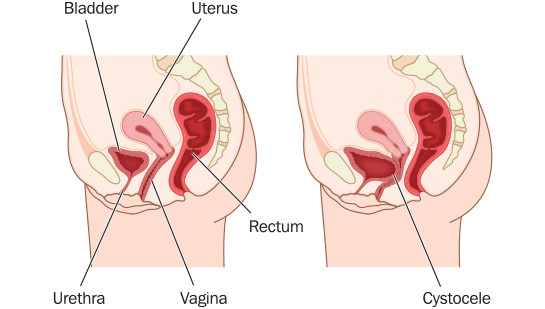
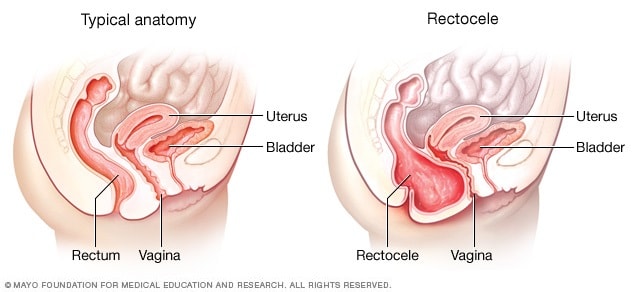
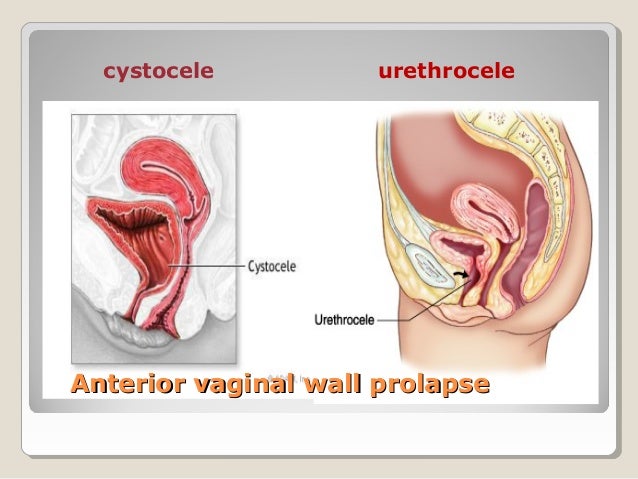
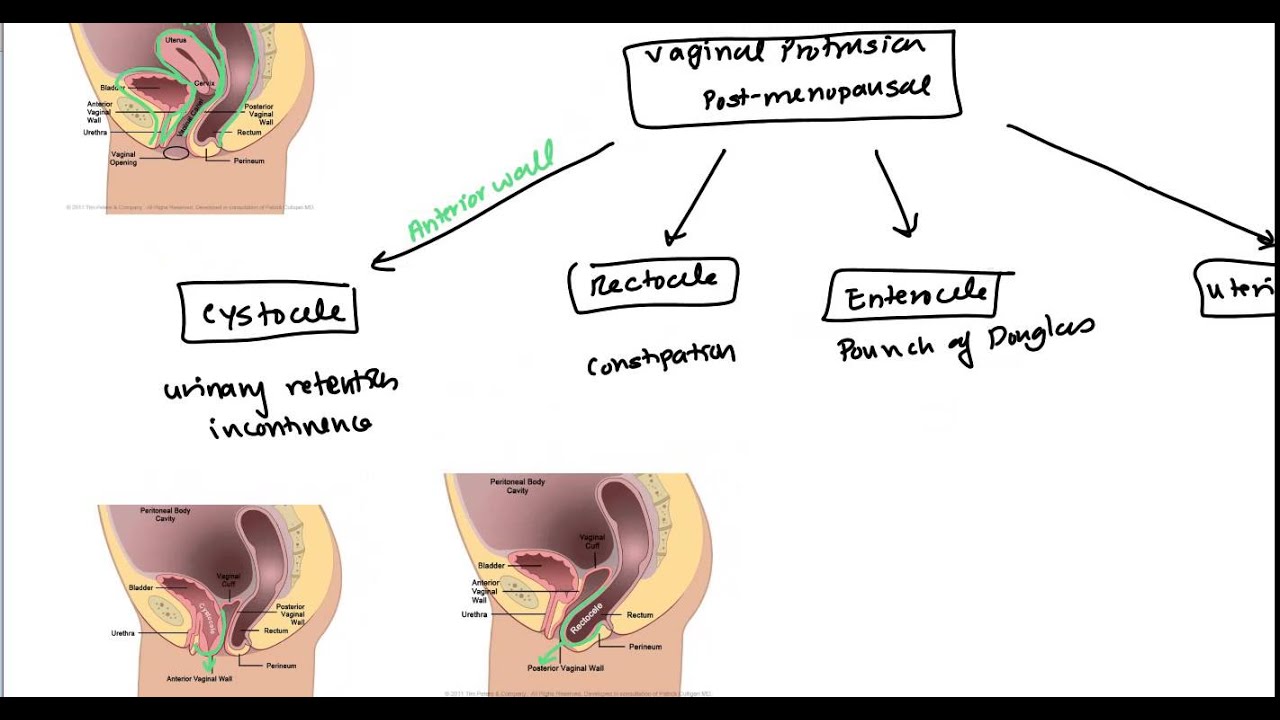
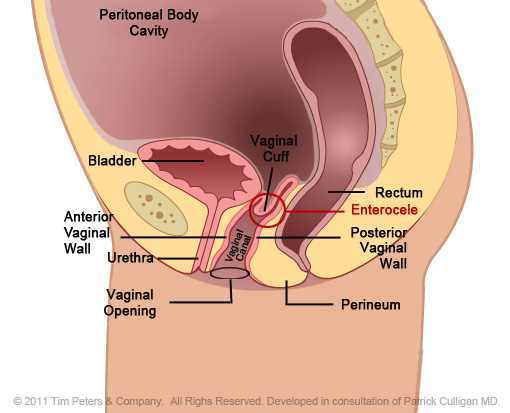
There are several different types of prolapse. Several of the organs in your pelvic area can shift out of place, developing into a prolapse. The different types of pelvic organ prolapse can include:
Vaginal prolapse is fairly common. More than one-third of women in the U.S. have some type of pelvic area prolapse during their lifetime. You’re more likely to experience a vaginal prolapse later in life, especially if you have had multiple pregnancies with a vaginal birth.
Your vagina is held in place within your pelvis by a group of muscles and other tissue—creating a support structure of sorts. This structure keeps the organs in your pelvis in place. Over time, this structure can weaken. When that happens, the vagina might slip down out of place, causing a prolapse. Several common causes of a vaginal prolapse can include:
Activities or conditions that place extra pressure on your abdominal area can also cause a prolapse. These can include:
In many cases, you may not feel any symptoms from a prolapse. You may find out about a vaginal prolapse during an exam in your healthcare provider’s office. If you do experience symptoms, they can include:
A vaginal prolapse is often diagnosed in your healthcare provider’s office during an appointment. Your provider will do a physical exam, talk to you about any symptoms of fullness in your pelvic area or urinary incontinence (leakage). You may also be asked about your family history and about any previous pregnancies.
In some cases, you may not have any symptoms and the prolapse could be found during a routine exam with your healthcare provider.
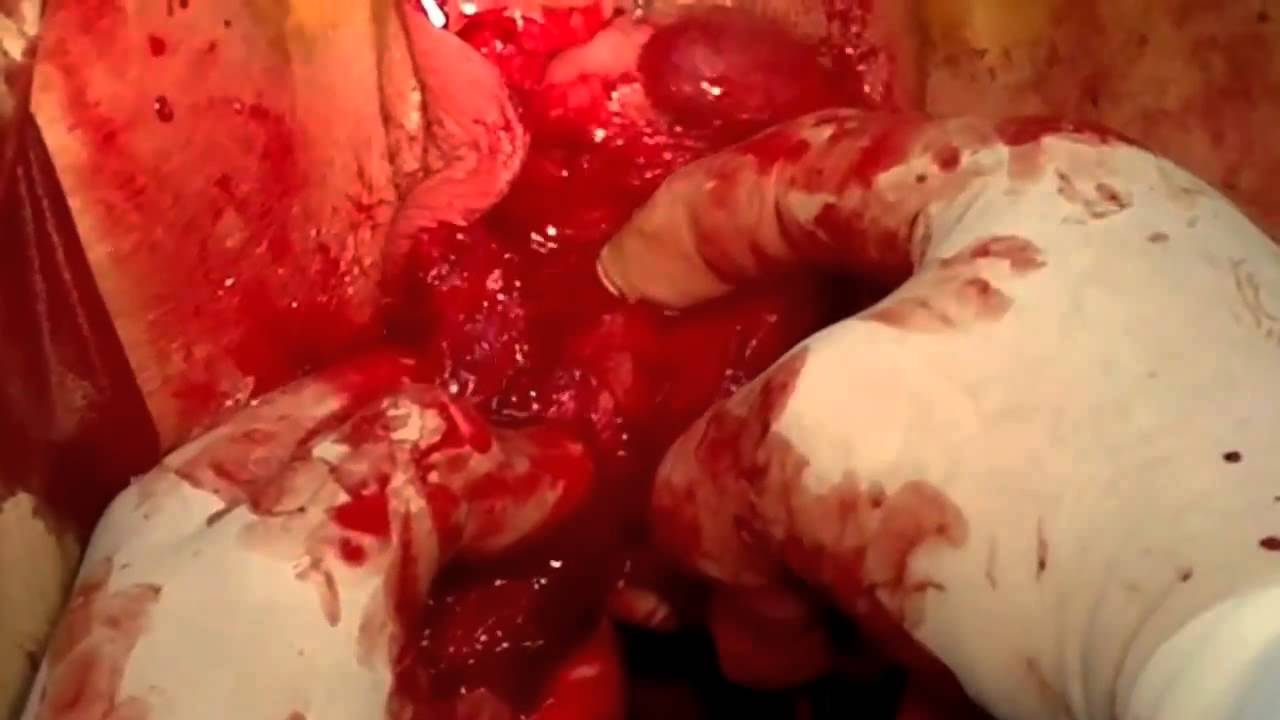
Treatment for vaginal prolapse can vary depending on the severity of your prolapse. In some cases, your healthcare provider may want to just watch it over time to make sure it doesn’t get worse.
There are non-surgical and surgical treatment options for vaginal prolapses. These treatments are very similar to treatment options for uterine prolapses. There are a few things your healthcare provider will take into account when forming a treatment plan. These can include:
It’s important to have an open and honest conversation with your healthcare provider about these topics. Some of the treatment options can mean no longer being able to become pregnant or have intercourse. Talk to your healthcare provider about any questions or concerns you have regarding these treatments.
Non-surgical treatments are typically used as a first option and work best with very minimal prolapses. Specific non-surgical treatment options can include:
Often, you can’t prevent a vaginal prolapse. There are good lifestyle habits you can adopt to decrease your risk of developing a vaginal prolapse. These can include:
When you lift something heavy, you can strain. This strain can lead to a prolapse. By following a few tips, you can lower your risk of prolapse.
A vaginal prolapse can happen again after treatment. However, most treatment plans are very successful. If you have multiple prolapses or a severe prolapse, your healthcare provider may talk to you about surgical treatment options.
In most cases, the outlook for a vaginal prolapse is positive. Treatment and lifestyle changes typically work well. Talk to your healthcare provider about all treatment options and what each option would mean for you. Your provider can help you develop good lifestyle habits that might help lower your risk of developing a vaginal prolapse in the future.
Last reviewed by a Cleveland Clinic medical professional on 12/30/2019.
Health Home
Conditions and Diseases
Robotic-Assisted Sacrocolpopexy
Uterine Prolapse
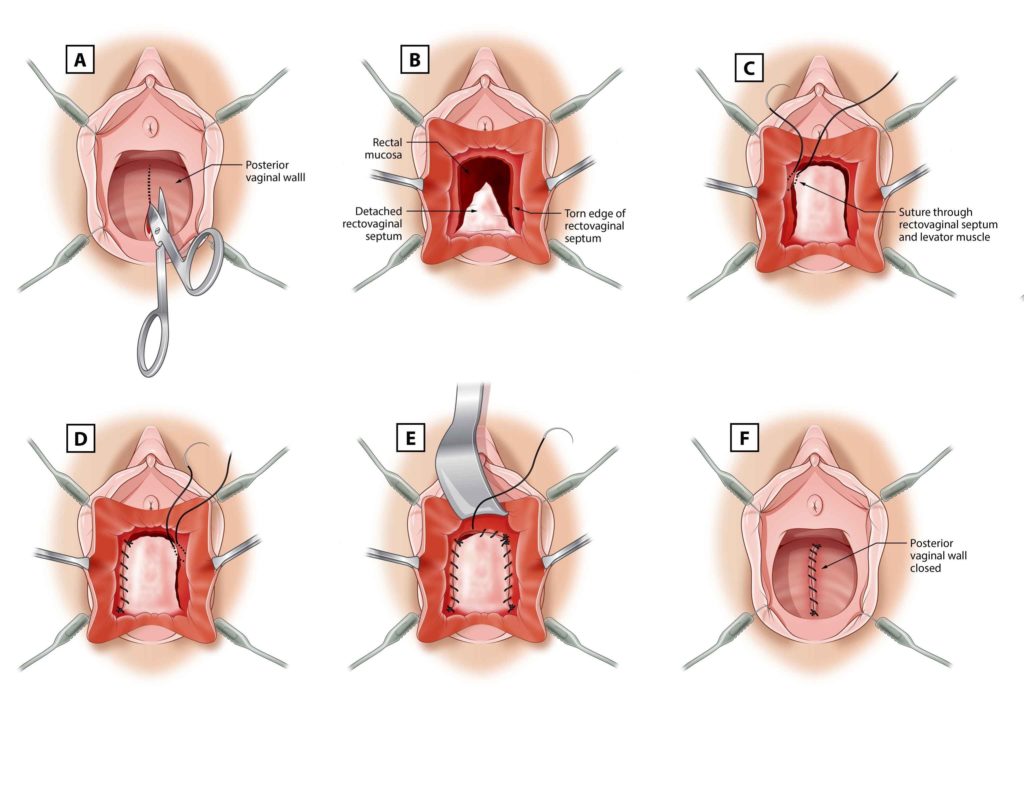
Rectocele
Request an Appointment
Find a Doctor
443-997-0400
Maryland
855-695-4872
Outside of Maryland
+1-410-502-7683
International
Health
Health Home
Conditions and Diseases
Treatments, Tests and Therapies
Wellness and Prevention
Caregiving
Language Assistance Available:
Español
አማርኛ
繁體中文
Français
Tagalog
Русский
Português
Italiano
Tiếng Việt
Ɓàsɔ́ɔ̀-wùɖù-po-nyɔ̀
Igbo asusu
èdè Yorùbá
বাংলা
日本語
한국어
Kreyòl Ayisyen
العربية
Deutsch
Polski
Ελληνικά
ગુજરાતી
ภาษาไทย
اُردُو
فارسی
हिंदी
Deitsch
ខ្មែរ
Copyright © 2021 The Johns Hopkins University, The Johns Hopkins Hospital, and Johns Hopkins Health System. All rights reserved.
Philips Respironics issued a recall for some CPAP and BiLevel PAP devices and mechanical ventilators. Learn more .
COVID-19 : We are vaccinating patients ages 12+. Learn more:
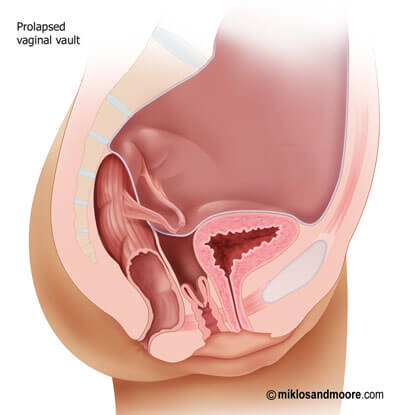
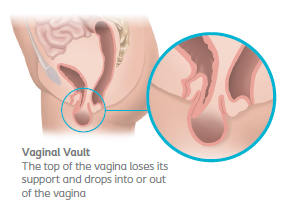
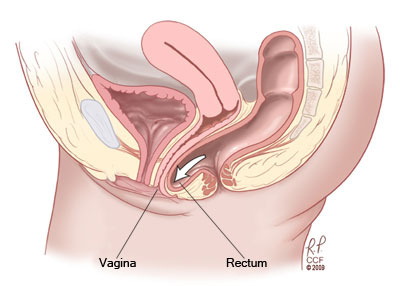
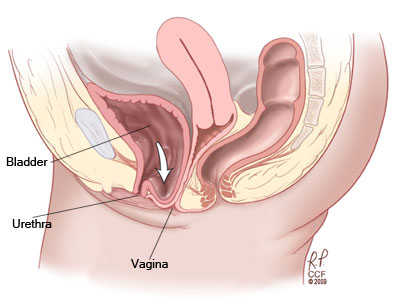
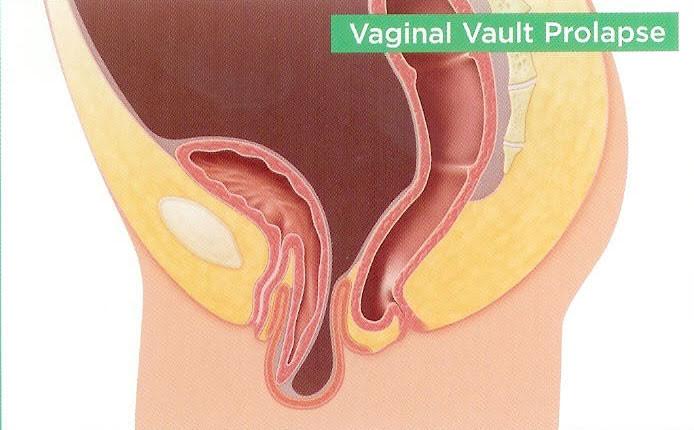
Prolapse occurs when a woman’s pelvic floor muscles, tissues and ligaments weaken and stretch. This can result in organs dropping out of their normal position. Vaginal prolapse refers to when the top of the vagina — also called the vaginal vault — sags and falls into the vaginal canal. In severe cases, the vagina can protrude outside of the body.
There are no direct causes of vaginal prolapse. However, women are at an increased risk of developing vaginal prolapse if they:
Hysterectomy, a surgery to remove a woman’s uterus, is sometimes performed to treat uterine prolapse. However, vaginal prolapse can occur after hysterectomy (regardless of the reason for hysterectomy). This is called “vaginal prolapse after hysterectomy.”
Vaginal prolapse is relatively common. About one-third of women will experience some degree of prolapse during their lifetime. If you have more than one risk factor, your chances of developing vaginal prolapse increase.
Women with vaginal prolapse often report feeling pressure in the vaginal area, described as a throbbing pain in the vagina. Women also report:
The pelvic organs are all supported by each other. When one organ prolapses, it can affect the functioning of other nearby organs. Thus, some women also experience:
Your doctor will review your medical and surgical history and complete a physical exam. Additional tests, such as ultrasound or MRI, are rarely needed. In some cases, your doctor may also recommended urodynamics testing, a group of tests that evaluate bladder function.
Our team of compassionate urogynecologists uses the latest research and advanced technologies to treat a range of pelvic floor disorders.
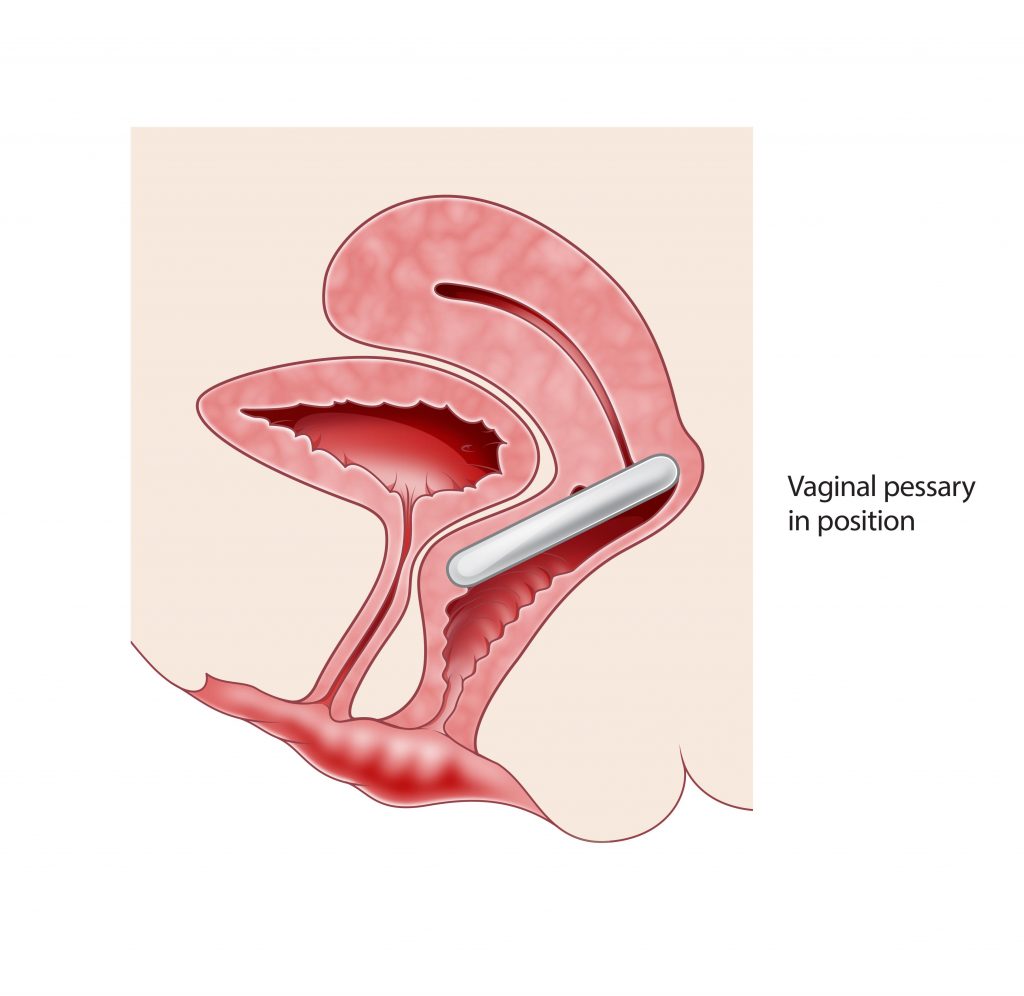
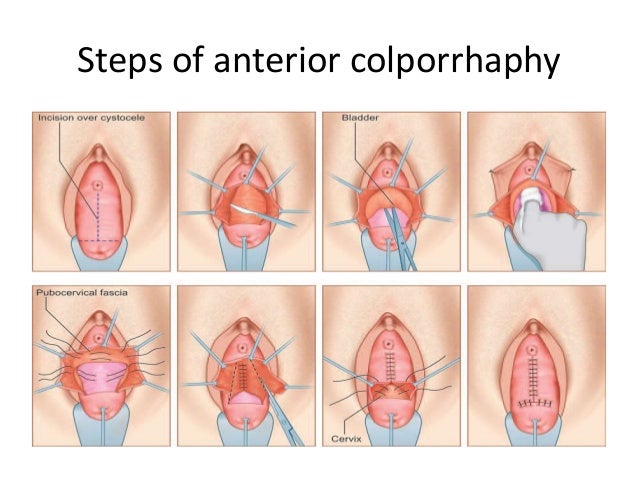
Treatment for vaginal prolapse varies, depending on the severity of the symptoms. Many cases will not require treatment. In mild cases, your physician may recommend pelvic floor exercises to strengthen the muscles. In moderate cases, your doctor may insert a vaginal pessary to support your vaginal wall. In the most severe cases, you may benefit from surgery, such as colposuspension , a minimally invasive surgical procedure, where the vaginal wall is attached to a stable ligament in the pelvis.
https://my.clevelandclinic.org/health/diseases/17597-vaginal-prolapse
https://www.hopkinsmedicine.org/health/conditions-and-diseases/vaginal-prolapse
Dude Licking Pussy
Porno Striptiz Club
Furry Trap Ass
Vaginal Prolapse: Symptoms, Causes, Treatments
Vaginal Prolapse | Johns Hopkins Medicine
Vaginal Prolapse: Symptoms, Treatment, Causes, and …
Vaginal Prolapse: What You Need to Know | …
Posterior vaginal prolapse (rectocele) - Symptoms …
Pelvic organ prolapse - NHS
Vaginal Prolapse (Wall/Vault): Symptoms, Causes, & …
What is a Vaginal Prolapse? (with pictures)
The Major Types of Pelvic Organ Prolapse and Their ...
Vaginal Prolapse