Vaginal Prolapse

🔞 ALL INFORMATION CLICK HERE 👈🏻👈🏻👈🏻
Vaginal Prolapse
Medically reviewed by Debra Rose Wilson, Ph.D., MSN, R.N., IBCLC, AHN-BC, CHT — Written by Stephanie Watson — Updated on September 18, 2018
Medically reviewed by Debra Rose Wilson, Ph.D., MSN, R.N., IBCLC, AHN-BC, CHT — Written by Stephanie Watson — Updated on September 18, 2018
Medically reviewed by Graham Rogers, M.D.
Medically reviewed by Carolyn Kay, MD
© 2005-2021 Healthline Media a Red Ventures Company. All rights reserved. Our website services, content, and products are for informational purposes only. Healthline Media does not provide medical advice, diagnosis, or treatment. See additional information .
© 2005-2021 Healthline Media a Red Ventures Company. All rights reserved. Our website services, content, and products are for informational purposes only. Healthline Media does not provide medical advice, diagnosis, or treatment. See additional information .
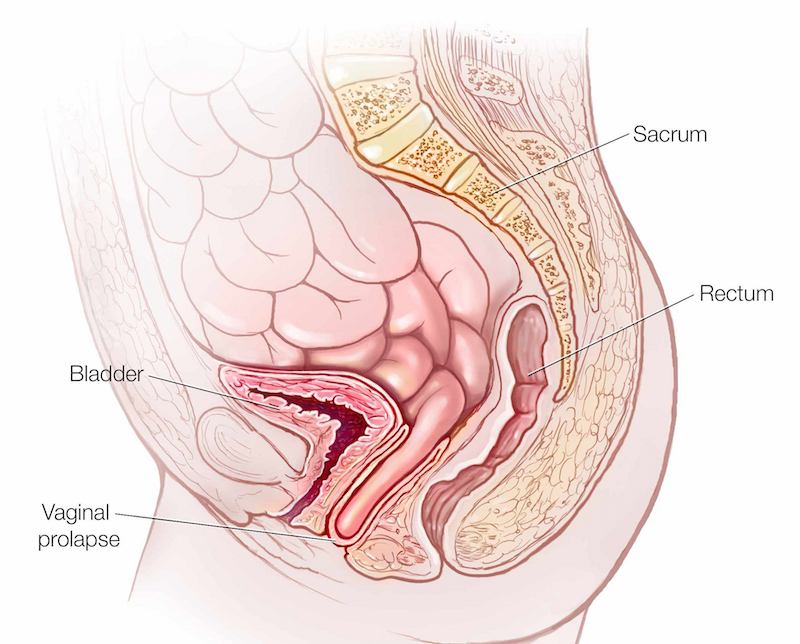
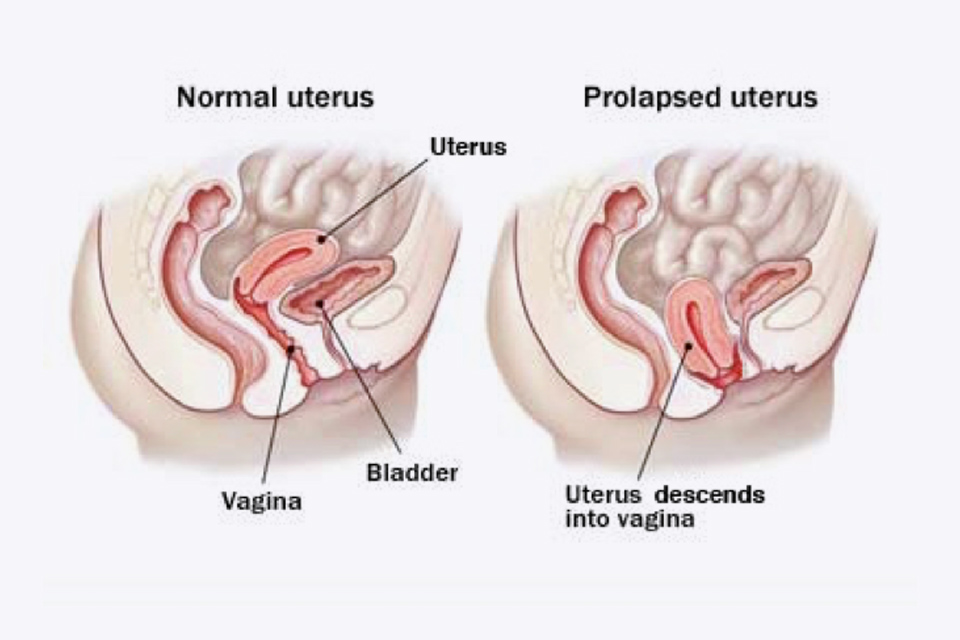
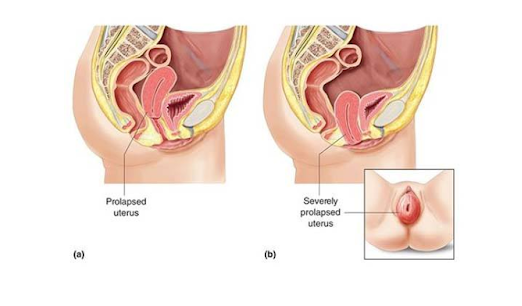
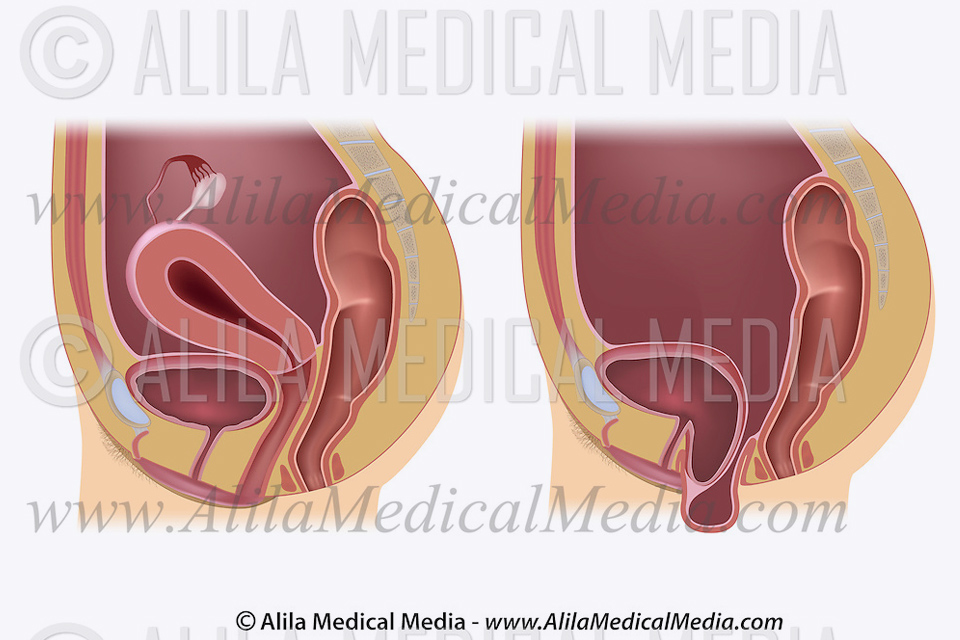
Vaginal prolapse happens when the muscles that support the organs in a woman’s pelvis weaken. This weakening allows the uterus, urethra, bladder, or rectum to droop down into the vagina. If the pelvic floor muscles weaken enough, these organs can even protrude out of the vagina.
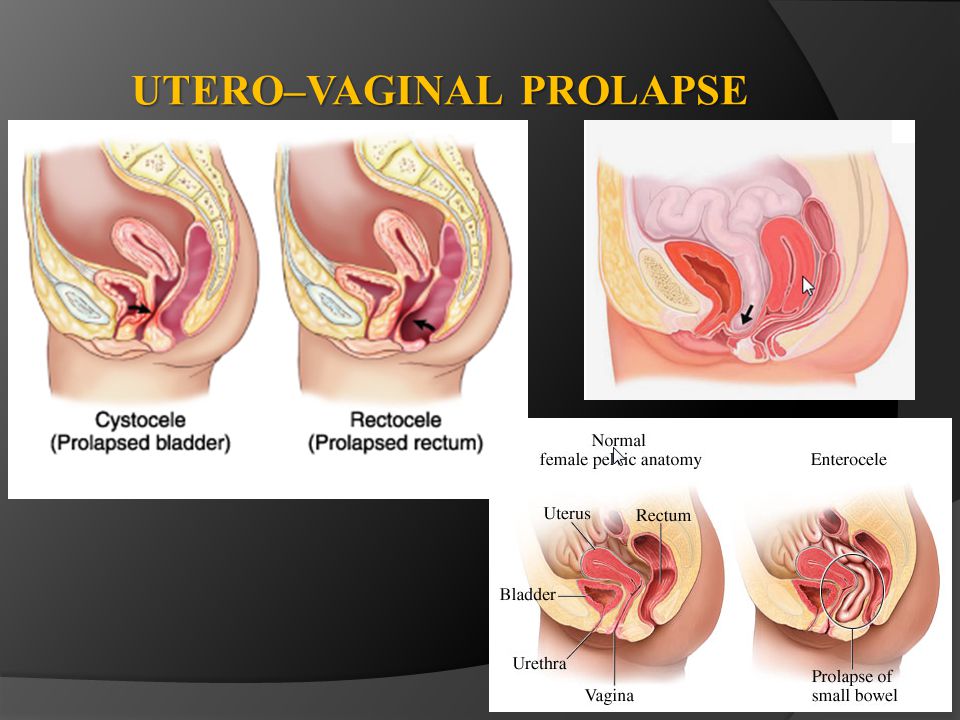
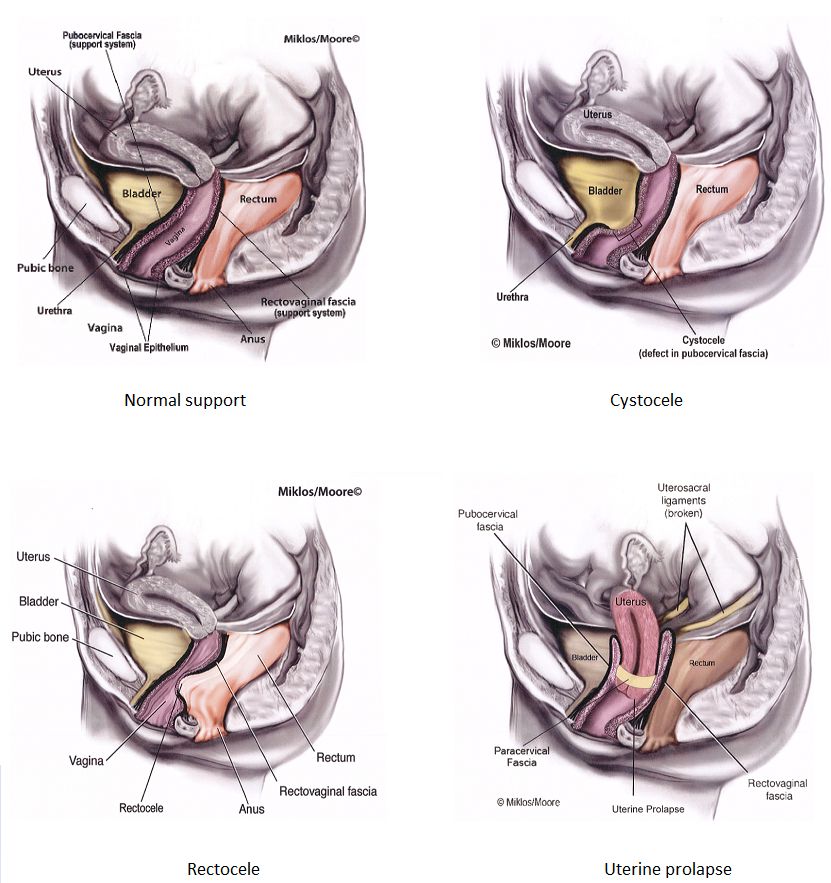
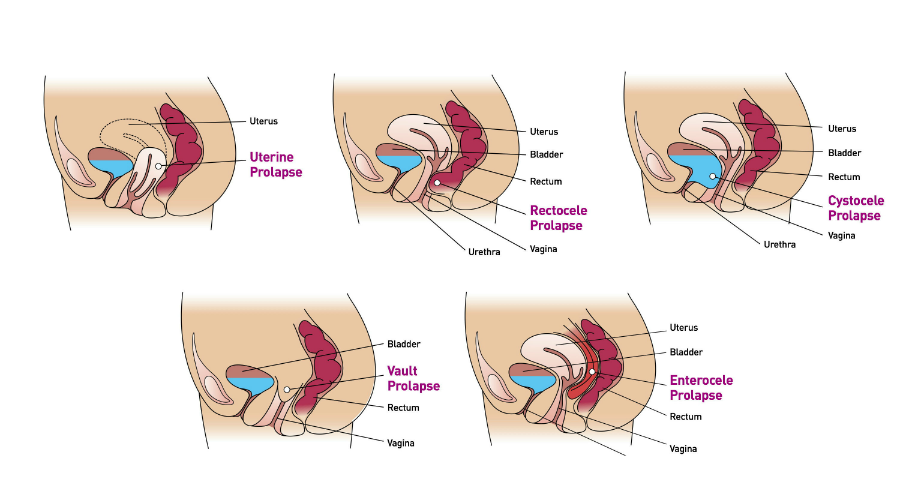
There are a few different types of prolapse:
Often women don’t have any symptoms from vaginal prolapse. If you do have symptoms, your symptoms will depend on the organ that is prolapsed.
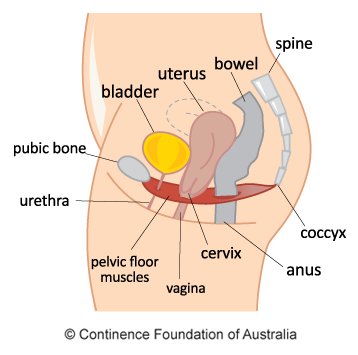
A hammock of muscles, called the pelvic floor muscles, supports your pelvic organs. Childbirth can stretch and weaken these muscles, especially if you had a difficult delivery.
Aging and the loss of estrogen during menopause can further weaken these muscles, allowing the pelvic organs to droop down into the vagina.
Other causes of vaginal prolapse include:
You’re more likely to have vaginal prolapse if you:
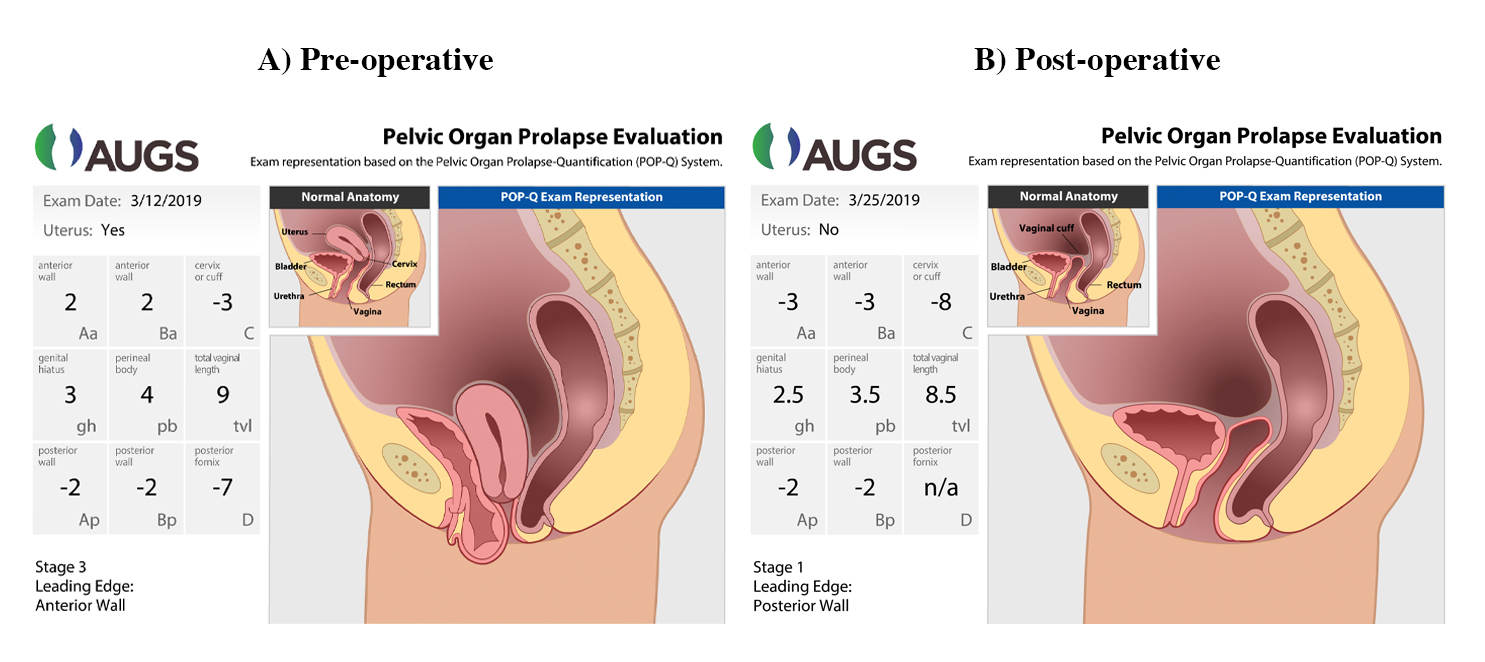
Vaginal prolapse can be diagnosed through a pelvic exam. During the exam, your doctor might ask you to bear down as if you’re trying to push out a bowel movement.
Your doctor might also ask you to tighten and release the muscles you’d use to stop and start the flow of urine. This test checks the strength of the muscles that support your vagina, uterus, and other pelvic organs.
If you have problems urinating, you may have tests to check your bladder function . This is called urodynamic testing.
Your doctor might also do one or more of these imaging tests to look for problems with your pelvic organs:
Your doctor will recommend the most conservative treatment methods first.
Pelvic floor exercises, also called Kegels , strengthen the muscles that support your vagina, bladder, and other pelvic organs. To do them:
To help learn where your pelvic floor muscles are, the next time you need to urinate, stop urinating midstream, then start again, and stop. Use this method to learn where the muscles are, it’s not meant to be a continued practice. In future practice, you can do this at times other than urinating. If you can’t find the right muscles, a physical therapist can use biofeedback to help you locate them.
Weight loss may also help. Losing excess weight can take some of the pressure off your bladder or other pelvic organs. Ask your doctor how much weight you need to lose.
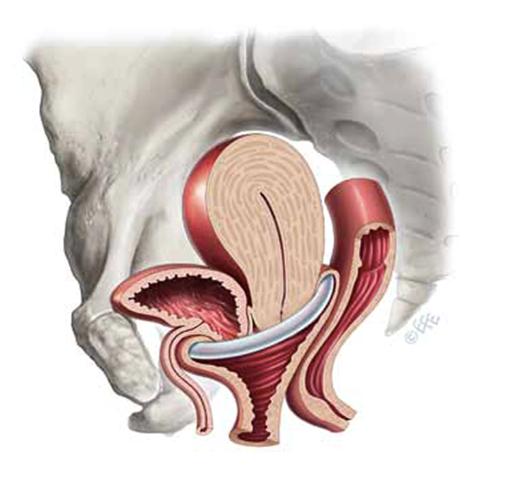
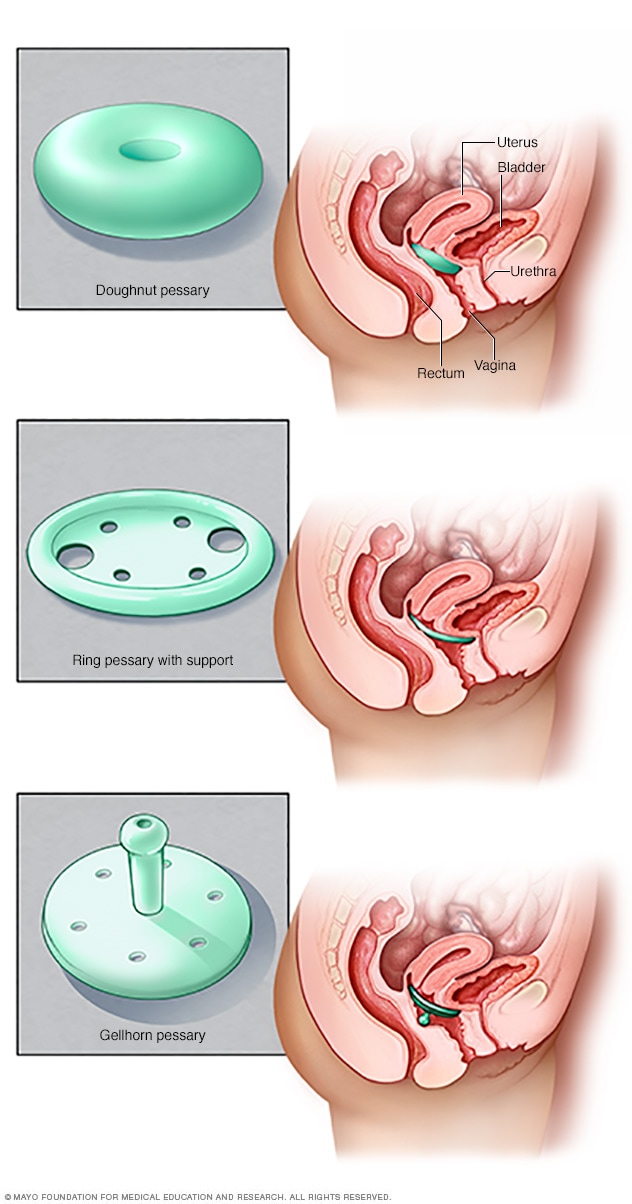
Another option is a pessary. This device, which is made from plastic or rubber, goes inside your vagina and holds the bulging tissues in place. It’s easy to learn how to insert a pessary and it helps avoid surgery.
If other methods don’t help, you may want to consider surgery to put the pelvic organs back in place and hold them there. A piece of your own tissue, tissue from a donor, or a man-made material will be used to support the weakened pelvic floor muscles. This surgery can be done through the vagina, or through small incisions (laparoscopically) in your abdomen.
Complications from vaginal prolapse depend on which organs are involved, but they can include:
If you have any symptoms of vaginal prolapse, including a feeling of fullness in your lower belly or a bulge in your vagina, see your gynecologist for an exam. This condition isn’t dangerous, but it can have a negative effect on your quality of life.
Vaginal prolapse is treatable. Milder cases can improve with noninvasive treatments like Kegel exercises and weight loss. For more severe cases, surgery can be effective. However, vaginal prolapse can sometimes come back after surgery.
Last medically reviewed on January 2, 2018
Vaginal prolapse : Causes and treatment options
Vaginal Prolapse : Symptoms, Treatment, Causes, and More
Vaginal Prolapse - Causes, Types, Pessary Device... | Everyday Health
Vaginal Prolapse – Causes, Symptoms and Treatment
vaginal prolapse - это... Что такое vaginal prolapse ?
Coronavirus Alert: February 25, 2021
FDA Watch: J&J Vaccine Okay Expected, COVID Spread Not Tied ...
Tippi Coronavirus: Tips for Living With COVID-19
Coronavirus and COVID-19: All Resources
Editorial Sources and Fact-Checking
Surgery for Pelvic Organ Prolapse; American Congress of Obstetricians and Gynecologists . Committee Opinion: Vaginal Placement of Synthetic Mesh for Pelvic Organ Prolapse (2011); Committee on Gynecologic Practice. R. G. Rogers and T. B. Fashokun (2016). "Pelvic organ prolapse in women: An overview of the epidemiology, risk factors, clinical manifestations, and management." UpToDate .
Wellness inspired. Wellness enabled.
Facebook Twitter Instagram Pinterest
© 1996-2021 Everyday Health, Inc. Everyday Health is among the federally registered trademarks of Everyday Health, Inc. and may not be used by third parties without explicit permission.
Learn what can cause the vagina and other pelvic organs to fall from their normal position.
Vaginal prolapse happens when the vagina falls from its normal location inside the pelvis toward the opening of the vagina.
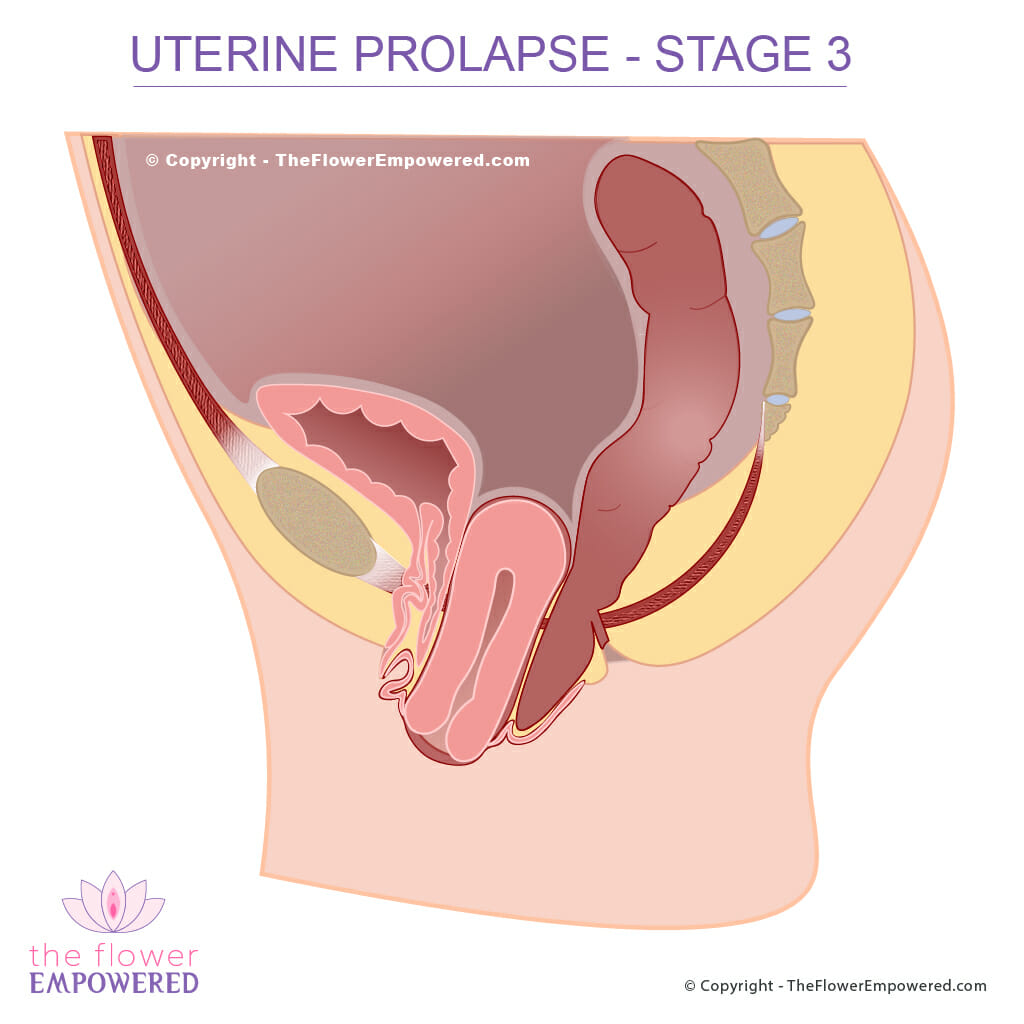
In severe cases of prolapse, the vagina may protrude outside the vaginal opening .
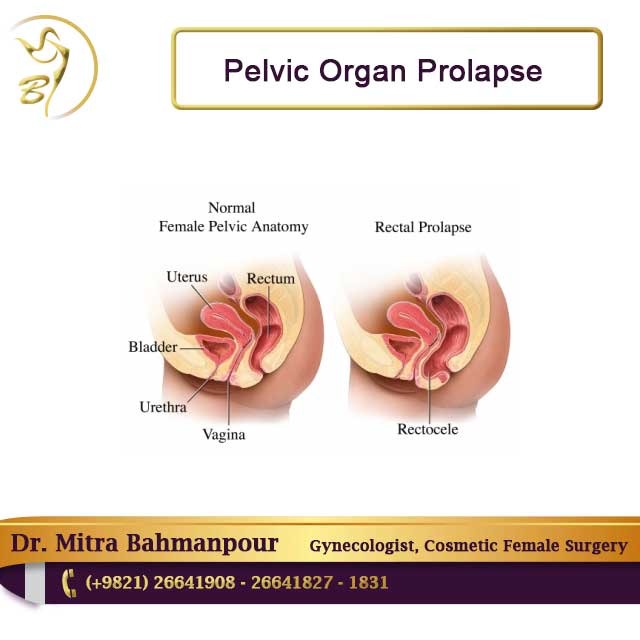
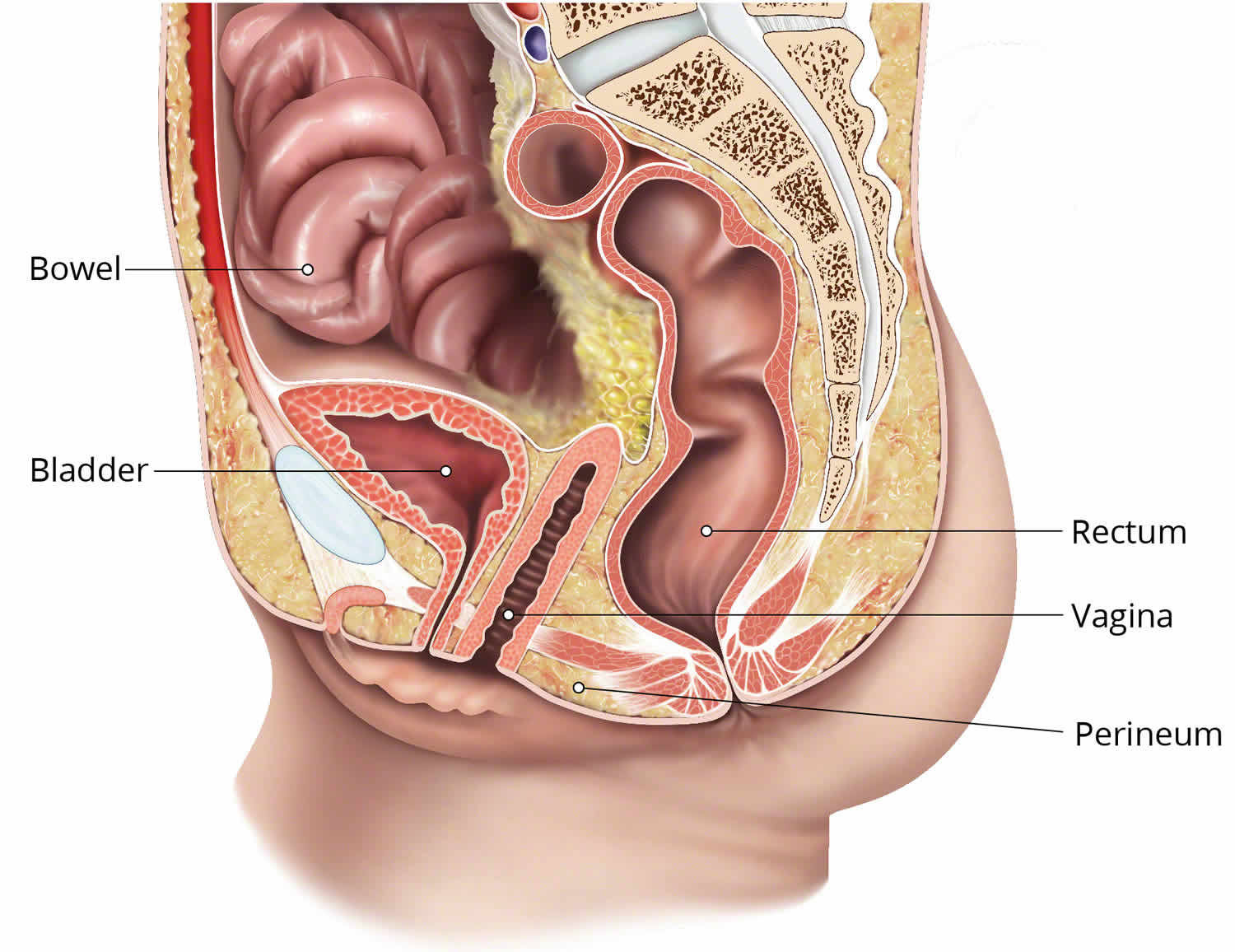
Vaginal prolapse seldom involves just the vagina. Other pelvic organs, including the uterus and bladder, can also fall out of place. This condition may be referred to, collectively, as pelvic organ prolapse.
The vagina and other pelvic organs are held in place by muscles and connective tissue. These muscles and tissues may become torn, stretched, or weakened.
Prolapse can happen when these muscles and tissues no longer adequately support the correct position of the pelvic organs.
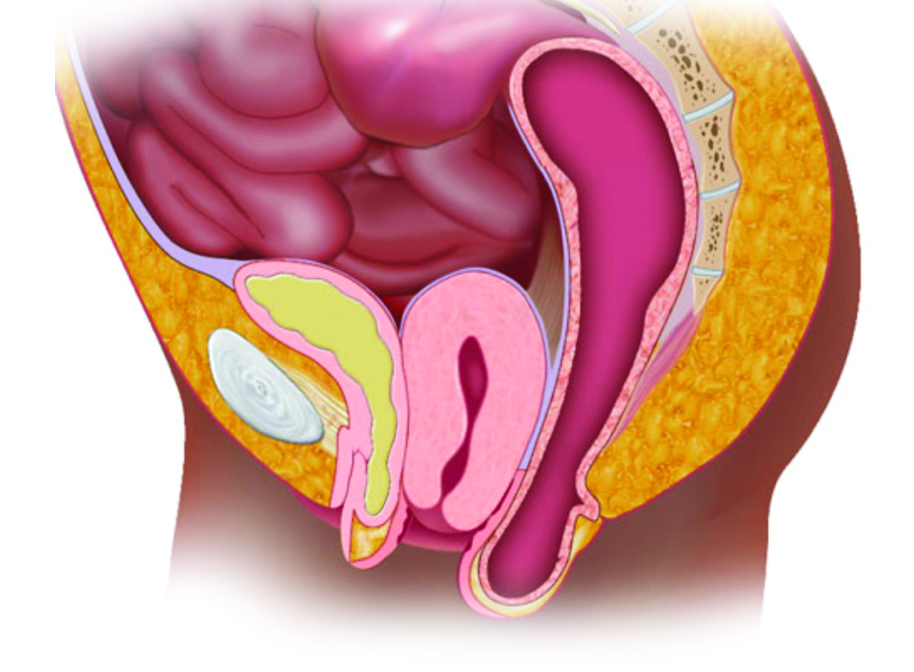
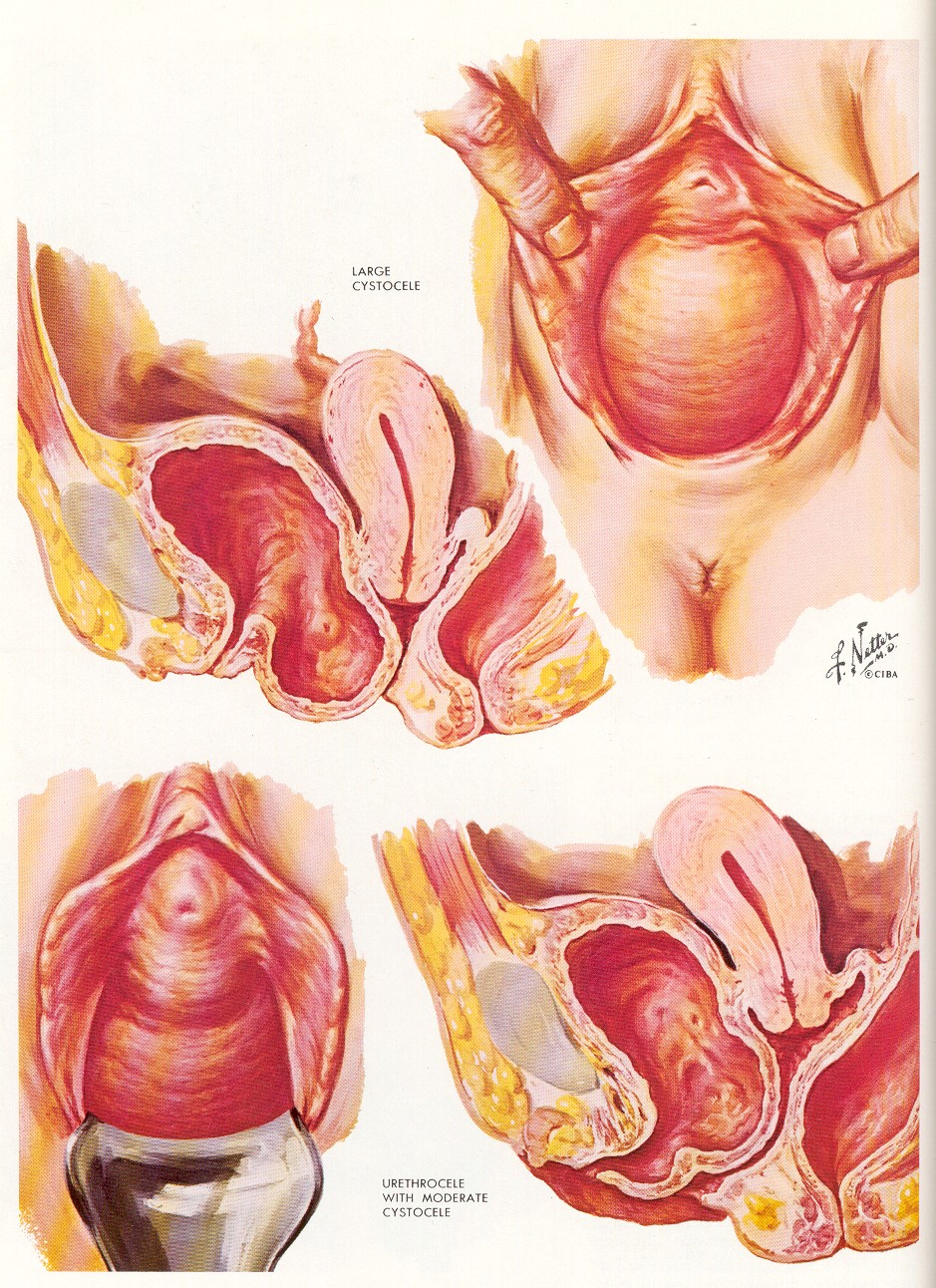
Different types of prolapse involve different parts of the female genitals:
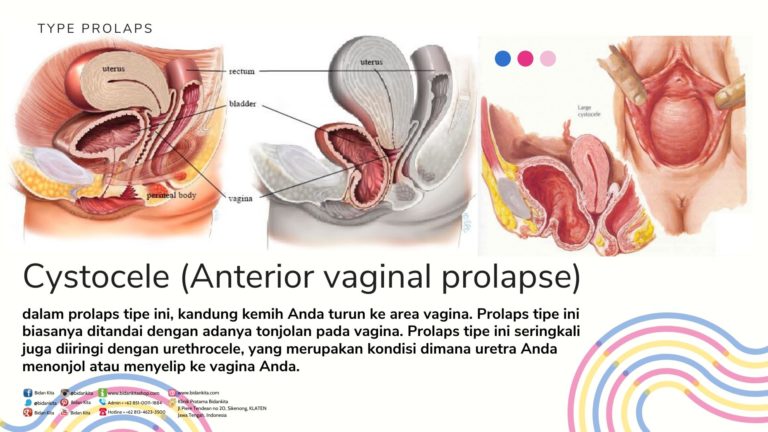
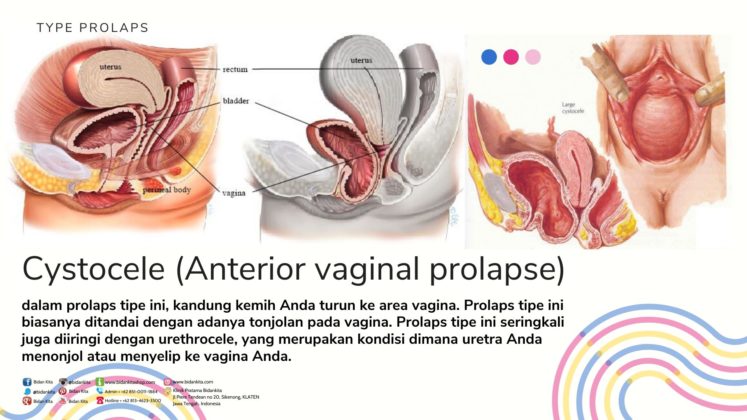
Cystocele This is when the bladder and front wall of the vagina sag toward the vaginal opening. It's sometimes called an anterior prolapse.
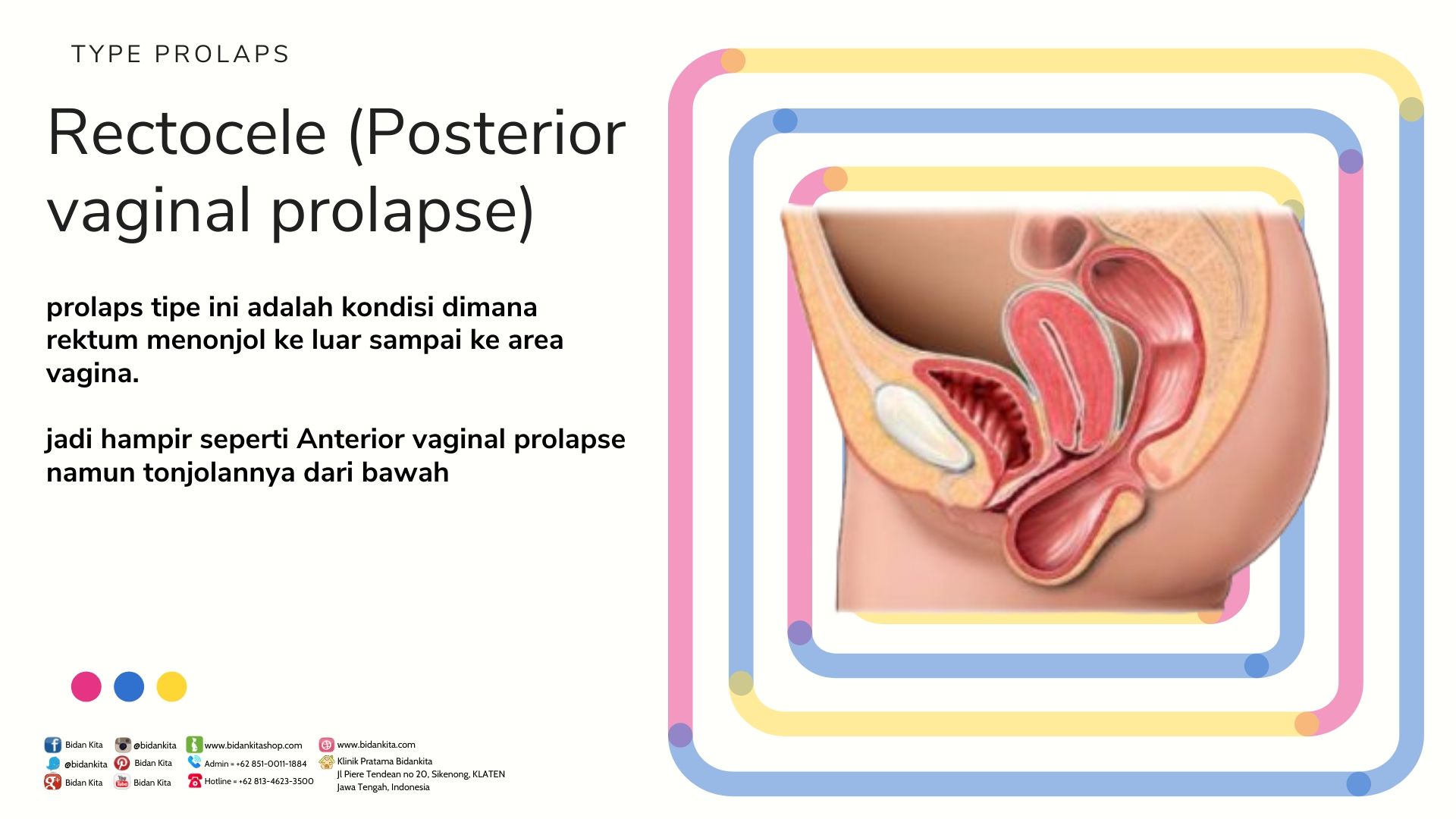
Rectocele This is when the rectum and back wall of the vagina fall downward toward the vaginal opening. It's sometimes called a posterior prolapse.
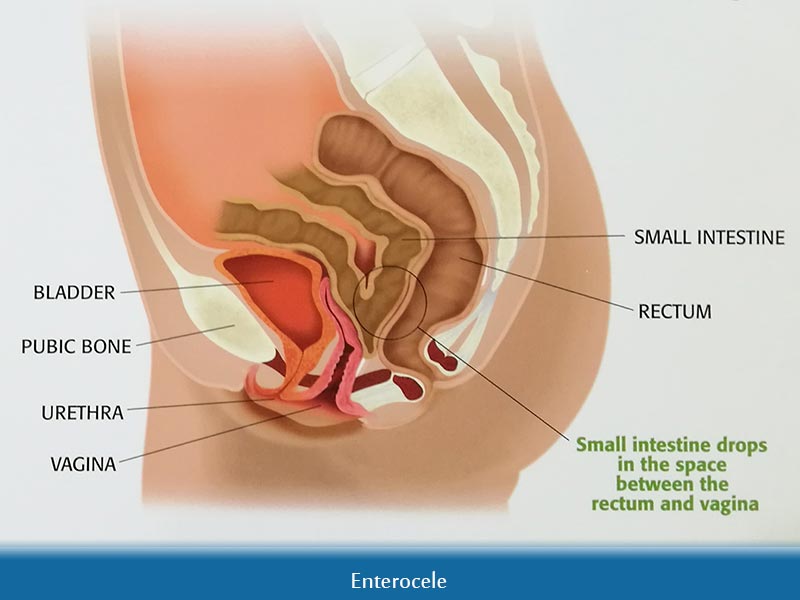
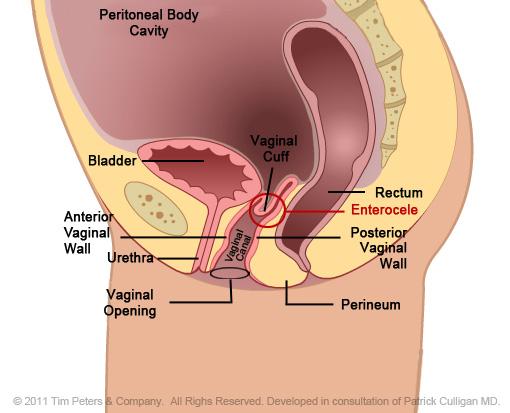
Enterocele This happens when the small bowel slips out of place. It can push down on the uterus or top of the vagina, causing these organs to fall toward the vaginal opening.
A vaginal pessary is the main nonsurgical treatment option for prolapse.
Pessaries are silicone devices that sit inside the vagina to hold the organs in place. They come in different shapes and sizes.
Your doctor will help you choose the pessary that's right for you based on your lifestyle, self-care abilities, and other factors.
Pessaries must be removed and cleaned on a regular basis. Some types of pessaries are easier than others to insert and remove at home.
If prolapse symptoms aren't resolved with a pessary or other nonsurgical treatments, your doctor may recommend surgery.
There are two main surgical approaches to fixing a vaginal prolapse.
One type of surgery involves narrowing or closing off the vagina to provide support for sagging organs.
Vaginal intercourse is no longer possible after this type of surgery.
In the other type of surgery, the surgeon will fix or suspend the sagging organs by repairing the pelvic muscles and tissues that support the pelvic organs.
If the muscles and tissues are too weak, surgical mesh can be used to hold the organs in place.
Transvaginal mesh is a material placed through the vagina during surgery to hold prolapsed organs in place.
There are a number of possible complications associated with transvaginal mesh, including:
Mesh erosion happens when the mesh moves through the wall of the vagina, where it can damage surrounding organs. Additional surgeries may be needed to fix this problem.
Surgery involving transvaginal mesh is typically reserved for women in whom previous repair attempts have failed, or whose own pelvic support tissues are too weak to repair.
By subscribing you agree to the Terms of Use and Privacy Policy .
New study also suggests that resilience to stressful events helps women manage hot flashes.
There’s a connection between endo and RA, according to a large study.
A diet with more fiber-rich fruits, vegetables, and whole grains may promote mental well-being in women, suggests new research.
New findings suggest that doctors who treat women have significant knowledge gaps that could compromise the care of this debilitating condition.
Racing heart, fluttering, and skipped heartbeats can be common before and during menopause transition.
By subscribing you agree to the Terms of Use and Privacy Policy .