Vagina Cervix

💣 👉🏻👉🏻👉🏻 ALL INFORMATION CLICK HERE 👈🏻👈🏻👈🏻
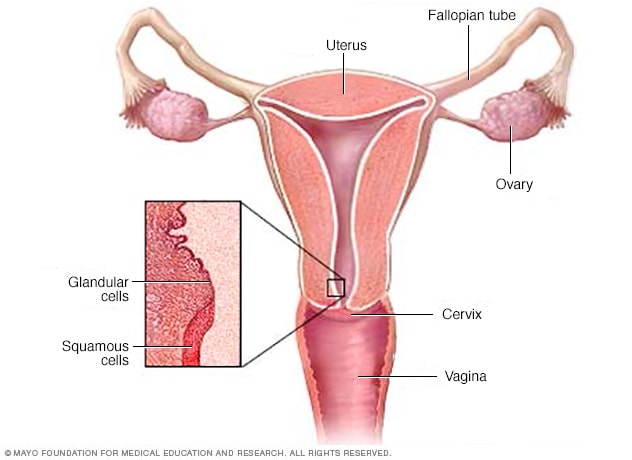
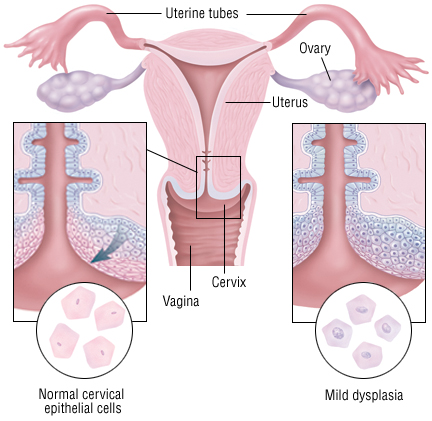
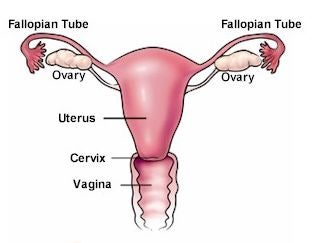
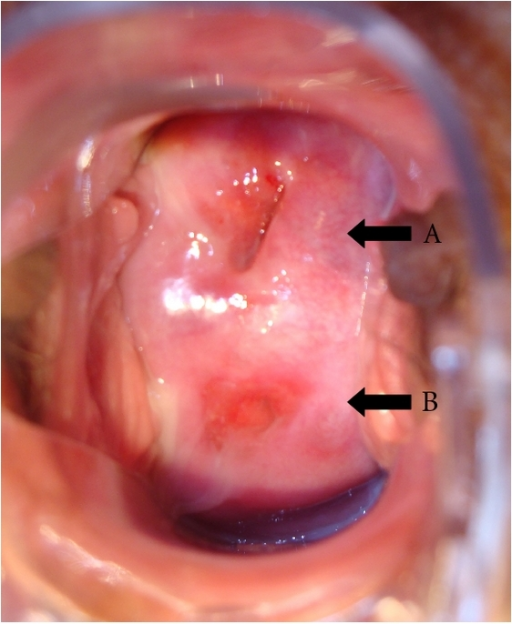
There are two main portions of the cervix:
www.webmd.com/women/picture-of-the …
https://www.webmd.com/women/picture-of-the-cervix
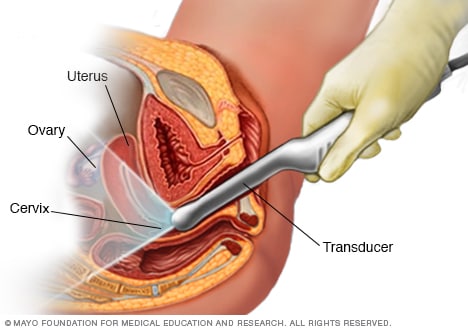
Перевести · 22.02.2012 · There are two main portions of the cervix: The part of the cervix that can be seen from inside the vagina during a gynecologic examination is known as the... The endocervix, or endocervical canal, is a tunnel through the cervix, from the external os into the uterus.
https://en.m.wikipedia.org/wiki/Cervix
The cervix is part of the female reproductive system. Around 2–3 centimetres (0.8–1.2 in) in length, it is the lower narrower part of the uterus continuous above with the broader upper part—or body—of the uterus. The lower end of the cervix bulges through the anterior wall of the vagina, and is referred to as the vaginal portion of cervix (or ectocervix) while the rest of the cervix above the vagina is called the supravaginal portion of cervix. A ce…
The cervix is part of the female reproductive system. Around 2–3 centimetres (0.8–1.2 in) in length, it is the lower narrower part of the uterus continuous above with the broader upper part—or body—of the uterus. The lower end of the cervix bulges through the anterior wall of the vagina, and is referred to as the vaginal portion of cervix (or ectocervix) while the rest of the cervix above the vagina is called the supravaginal portion of cervix. A central canal, known as the cervical canal, runs along its length and connects the cavity of the body of the uterus with the lumen of the vagina. The openings are known as the internal os and external orifice of the uterus (or external os) respectively. The mucosa lining the cervical canal is known as the endocervix, and the mucosa covering the ectocervix is known as the exocervix. The cervix has an inner mucosal layer, a thick layer of smooth muscle, and posteriorly the supravaginal portion has a serosal covering consisting of connective tissue and overlying peritoneum.
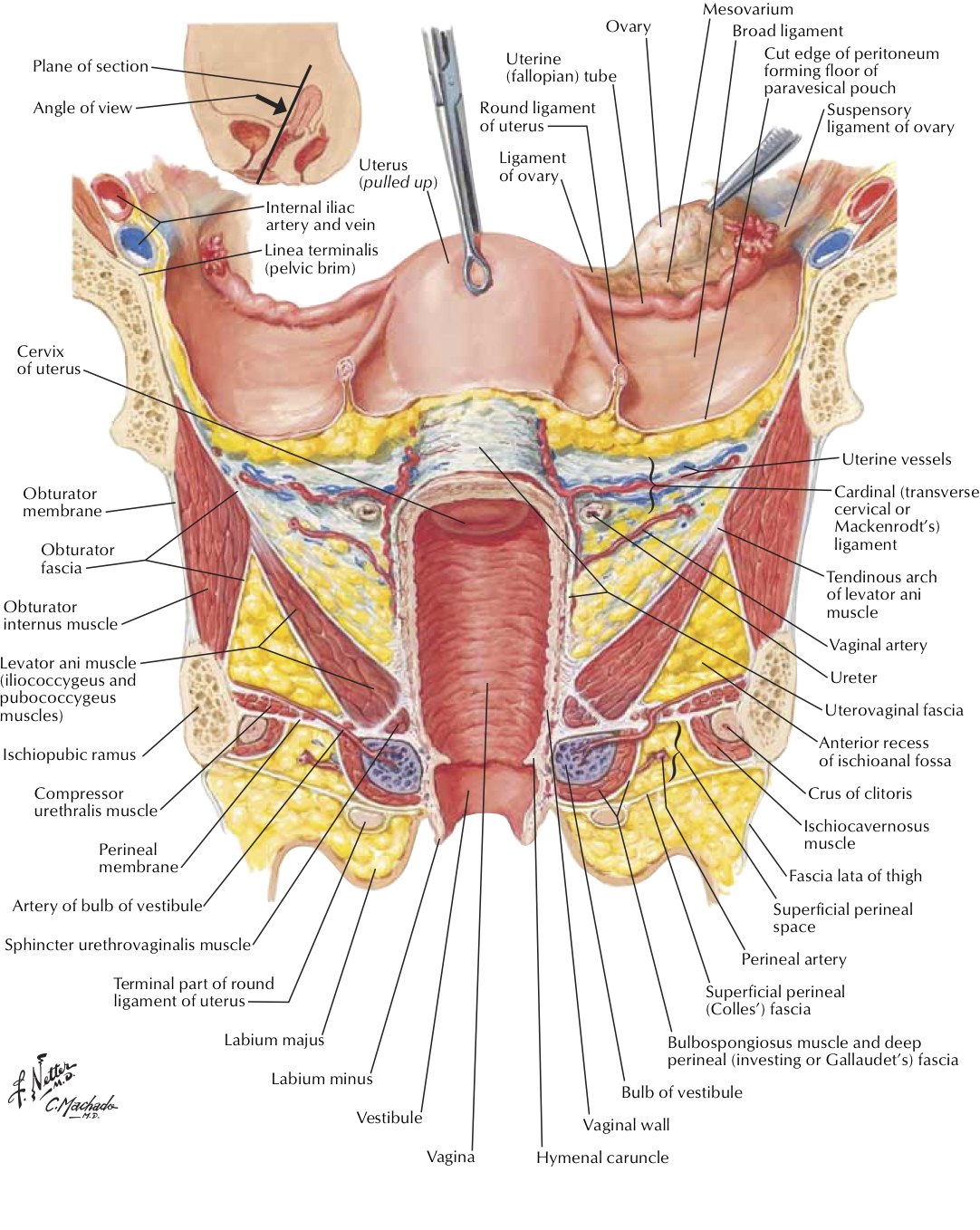
In front of the upper part of the cervix lies the bladder, separated from it by cellular connective tissue known as parametrium, which also extends over the sides of the cervix. To the rear, the supravaginal cervix is covered by peritoneum, which runs onto the back of the vaginal wall and then turns upwards and onto the rectum, forming the recto-uterine pouch. The cervix is more tightly connected to surrounding structures than the rest of the uterus.
The cervical canal varies greatly in length and width between women or over the course of a woman's life, and it can measure 8 mm (0.3 inch) at its widest diameter in premenopausal adults. It is wider in the middle and narrower at each end. The anterior and posterior walls of the canal each have a vertical fold, from which ridges run diagonally upwards and laterally. These are known as palmate folds, due to their resemblance to a palm leaf. The anterior and posterior ridges are arranged in such a way that they interlock with each other and close the canal. They are often effaced after pregnancy.
The ectocervix (also known as the vaginal portion of the cervix) has a convex, elliptical shape and projects into the cervix between the anterior and posterior vaginal fornices. On the rounded part of the ectocervix is a small, depressed external opening, connecting the cervix with the vagina. The size and shape of the ectocervix and the external opening (external os) can vary according to age, hormonal state, and whether natural or normal childbirth has taken place. In women who have not had a vaginal delivery, the external opening is small and circular, and in women who have had a vaginal delivery, it is slit-like. On average, the ectocervix is 3 cm (1.2 in) long and 2.5 cm (1 in) wide.
Blood is supplied to the cervix by the descending branch of the uterine artery and drains into the uterine vein. The pelvic splanchnic nerves, emerging as S2–S3, transmit the sensation of pain from the cervix to the brain. These nerves travel along the uterosacral ligaments, which pass from the uterus to the anterior sacrum.
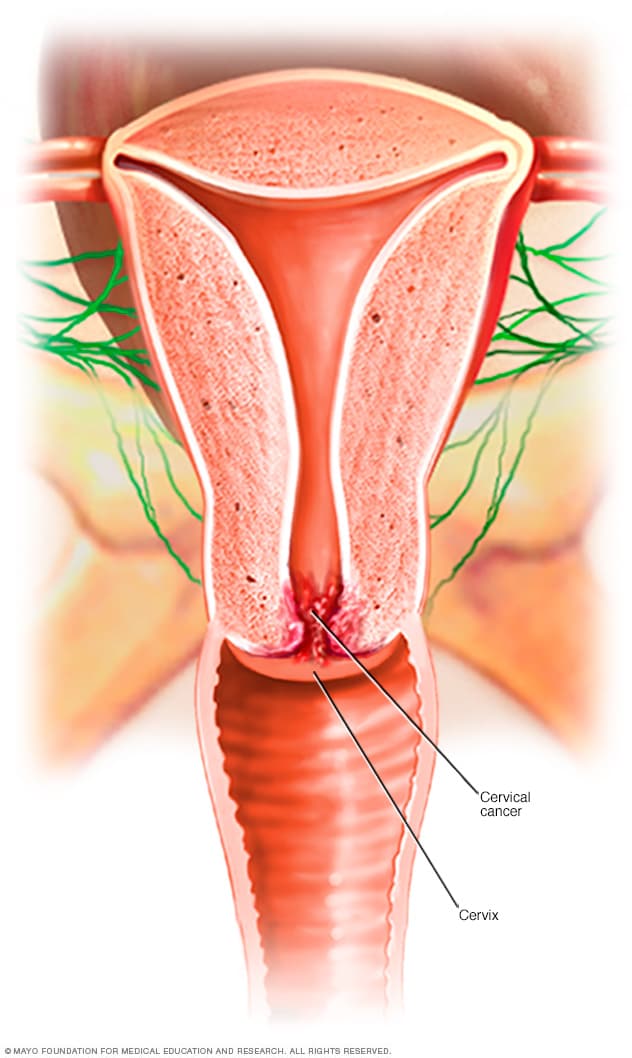
Three channels facilitate lymphatic drainage from the cervix. The anterior and lateral cervix drains to nodes along the uterine arteries, travelling along the cardinal ligaments at the base of the broad ligament to the external iliac lymph nodes and ultimately the paraaortic lymph nodes. The posterior and lateral cervix drains along the uterine arteries to the internal iliac lymph nodes and ultimately the paraaortic lymph nodes, and the posterior section of the cervix drains to the obturator and presacral lymph nodes. However, there are variations as lymphatic drainage from the cervix travels to different sets of pelvic nodes in some people. This has implications in scanning nodes for involvement in cervical cancer.
After menstruation and directly under the influence of estrogen, the cervix undergoes a series of changes in position and texture. During most of the menstrual cycle, the cervix remains firm, and is positioned low and closed. However, as ovulation approaches, the cervix becomes softer and rises to open in response to the higher levels of estrogen present. These changes are also accompanied by changes in cervical mucus, described below.
Development
As a component of the female reproductive system, the cervix is derived from the two paramesonephric ducts (also called Müllerian ducts), which develop around the sixth week of embryogenesis. During development, the outer parts of the two ducts fuse, forming a single urogenital canal that will become the vagina, cervix and uterus. The cervix grows in size at a smaller rate than the body of the uterus, so the relative size of the cervix over time decreases, decreasing from being much larger than the body of the uterus in fetal life, twice as large during childhood, and decreasing to its adult size, smaller than the uterus, after puberty. Previously it was thought that during fetal development, the original squamous epithelium of the cervix is derived from the urogenital sinus and the original columnar epithelium is derived from the paramesonephric duct. The point at which these two original epithelia meet is called the original squamocolumnar junction. New studies show, however, that all the cervical as well as large part of the vaginal epithelium are derived from Müllerian duct tissue and that phenotypic differences might be due to other causes.
Histology
The endocervical mucosa is about 3 mm (0.12 in) thick and lined with a single layer of columnar mucous cells. It contains numerous tubular mucous glands, which empty viscous alkaline mucus into the lumen. In contrast, the ectocervix is covered with nonkeratinized stratified squamous epithelium, which resembles the squamous epithelium lining the vagina. The junction between these two types of epithelia is called the squamocolumnar junction. Underlying both types of epithelium is a tough layer of collagen. The mucosa of the endocervix is not shed during menstruation. The cervix has more fibrous tissue, including collagen and elastin, than the rest of the uterus.
In prepubertal girls, the functional squamocolumnar junction is present just within the cervical canal. Upon entering puberty, due to hormonal influence, and during pregnancy, the columnar epithelium extends outward over the ectocervix as the cervix everts. Hence, this also causes the squamocolumnar junction to move outwards onto the vaginal portion of the cervix, where it is exposed to the acidic vaginal environment. The exposed columnar epithelium can undergo physiological metaplasia and change to tougher metaplastic squamous epithelium in days or weeks, which is very similar to the original squamous epithelium when mature. The new squamocolumnar junction is therefore internal to the original squamocolumnar junction, and the zone of unstable epithelium between the two junctions is called the transformation zone of the cervix. Histologically, the transformation zone is generally defined as surface squamous epithelium with surface columnar epithelium or stromal glands/crypts, or both.
After menopause, the uterine structures involute and the functional squamocolumnar junction moves into the cervical canal.
Nabothian cysts (or Nabothian follicles) form in the transformation zone where the lining of metaplastic epithelium has replaced mucous epithelium and caused a strangulation of the outlet of some of the mucous glands. A buildup of mucus in the glands forms Nabothian cysts, usually less than about 5 mm (0.20 in) in diameter, which are considered physiological rather than pathological. Both gland openings and Nabothian cysts are helpful to identify the transformation zone.
https://pathology.oit.duke.edu/siteParts/avaps/05.31.2_Pathology_of_the_Female...
Vagina . Ectroprion is a completely normal finding in younger women. Often mistaken for cervical neoplasia. Junction hidden from view. In younger women, the dndocervical …
https://helloclue.com/articles/cycle-a-z/how-to-find-feel-your-cervix
Перевести · 01.12.2016 · In the vagina, the cervix looks like a smooth fleshy O, about an inch or 2.5cm in diameter, with a hole in the middle — similar to puckered lips. Your cervix …
Как довести девушку до оргазма Стимуляция точки G
How To Use Cervical Cap? - Manipal Hospital
Conception 101: How To Find Your Cervix
Влага́лище — конечный отдел половых проводящих путей у самок млекопитающих. Влагалище служит для полового сношения, также через него осуществляются роды.
Система: Репродуктивная и мочевыделительная
Кровоснабжение: внутренняя подвздошная артерия, нисходящая ветвь маточной артерии, нижняя пузырная артерия, средняя прямокише…
Венозный отток: влагалищное венозное сплетение
Иннервация: верхнее подчревное сплетение, правые и левые нижние подчревные сплетения, тазовый нерв
Лимфа: поверхностные и глубокие паховые лимфоузлы, лимфоузлов малого таза
https://www.wikihow.com/Feel-Your-Cervix
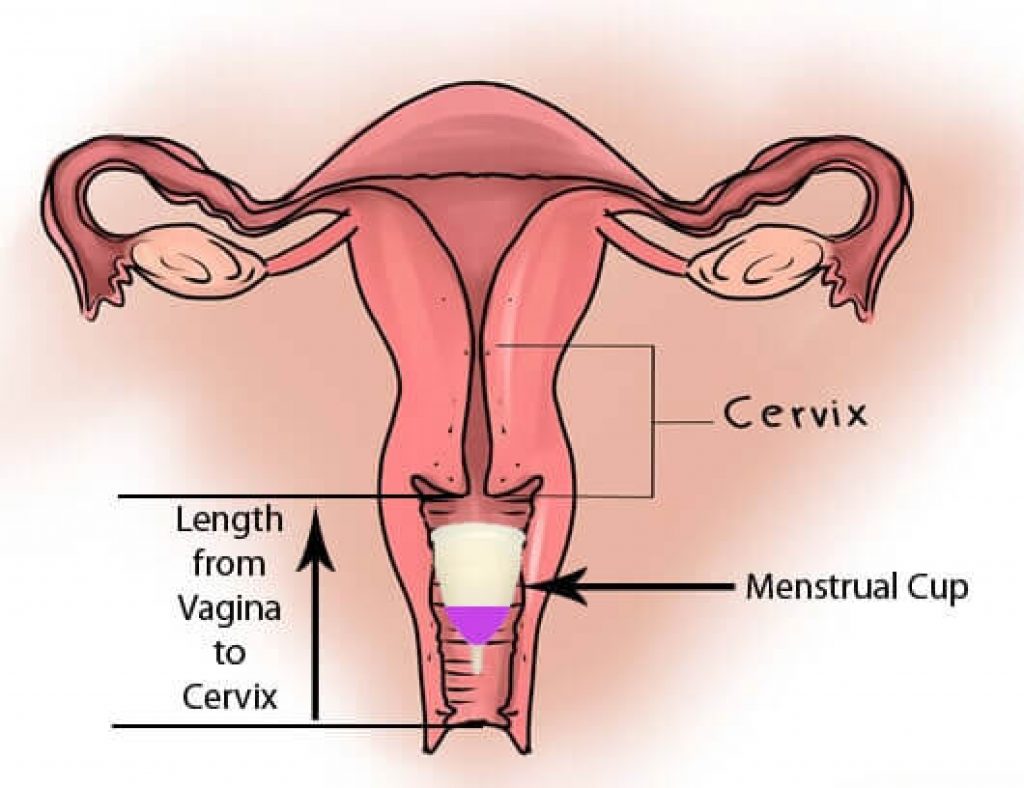
Know where your cervix is located. The cervix is the lowermost part of the uterus, where it connects with the vaginal wall.[1] X Trustworthy Source MedlinePlus Collection of medical information sourced from the US National Library of Medicine Go to source It is located 3 to 6 inches (7.6 to 15.2 cm) inside the vagina, at the end of the vaginal tunnel. It is shaped like …
Wash your hands with soap and warm water. Si…
https://www.healthline.com/health/womens-health/cervix-penetration
Перевести · 26.07.2017 · Your cervix starts at the base of your uterus and stretches to your vagina. Think of it like a neck made of tissue that connects the two parts. What your gyno sees during a …
https://en.m.wikipedia.org/wiki/Vaginal
Artery: superior part to uterine artery, middle and …
Precursor: urogenital sinus and paramesonephric …
Vein: uterovaginal venous plexus, vaginal vein
Nerve: Sympathetic: lumbar splanchnic plexus, Parasympathetic: pelvic splanchnic plexus
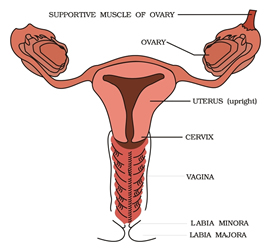
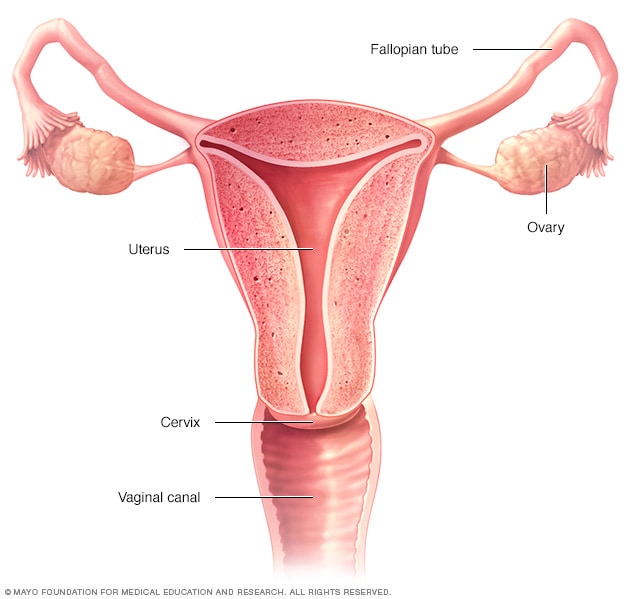
In mammals, the vagina is the elastic, muscular part of the female genital tract. In humans, it extends from the vulva to the cervix. The outer vaginal opening is normally partly covered by a membrane called the hymen. At the deep end, the cervix (neck of the uterus) bulges into the vagina. The vagina allows for sexual intercourse and birth. It also channels menstrual flow (menses), which occurs in humans and closely related primates as part of the monthly menstrual cycle.
In mammals, the vagina is the elastic, muscular part of the female genital tract. In humans, it extends from the vulva to the cervix. The outer vaginal opening is normally partly covered by a membrane called the hymen. At the deep end, the cervix (neck of the uterus) bulges into the vagina. The vagina allows for sexual intercourse and birth. It also channels menstrual flow (menses), which occurs in humans and closely related primates as part of the monthly menstrual cycle.
Although research on the vagina is especially lacking for different animals, its location, structure and size are documented as varying among species. Female mammals usually have two external openings in the vulva, the urethral opening for the urinary tract and the vaginal opening for the genital tract. This is different from male mammals, who usually have a single urethral opening for both urination and reproduction. The vaginal opening is much larger than the nearby urethral opening, and both are protected by the labia in humans. In amphibians, birds, reptiles and monotremes, the cloaca is the single external opening for the gastrointestinal tract, the urinary, and reproductive tracts.
To accommodate smoother penetration of the vagina during sexual intercourse or other sexual activity, vaginal moisture increases during sexual arousal in human females and other female mammals. This increase in moisture provides vaginal lubrication, which reduces friction. The texture of the vaginal walls creates friction for the penis during sexual intercourse and stimulates it toward ejaculation, enabling fertilization. Along with pleasure and bonding, women's sexual behavior with others (which can include heterosexual or lesbian sexual activity) can result in sexually transmitted infections (STIs), the risk of which can be reduced by recommended safe sex practices. Other health issues may also affect the human vagina.
The vagina and vulva have evoked strong reactions in societies throughout history, including negative perceptions and language, cultural taboos, and their use as symbols for female sexuality, spirituality, or regeneration of life. In common speech, the word vagina is often used to refer to the vulva or to the female genitals in general. By its dictionary and anatomical definitions, however, vagina refers exclusively to the specific internal structure, and understanding the distinction can improve knowledge of the female genitalia and aid in healthcare communication.
Влагалищная часть шейки матки — внешняя часть матки, которая полусферой вдаётся в за…
Не удается получить доступ к вашему текущему расположению. Для получения лучших результатов предоставьте Bing доступ к данным о расположении или введите расположение.
Не удается получить доступ к расположению вашего устройства. Для получения лучших результатов введите расположение.
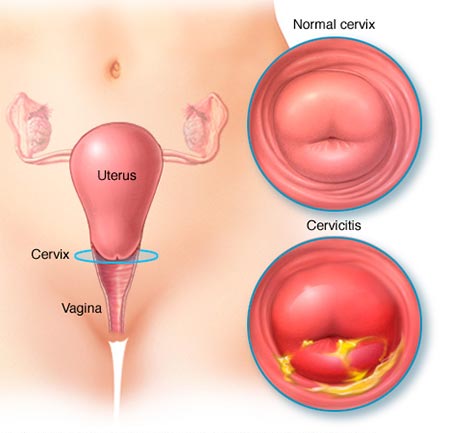
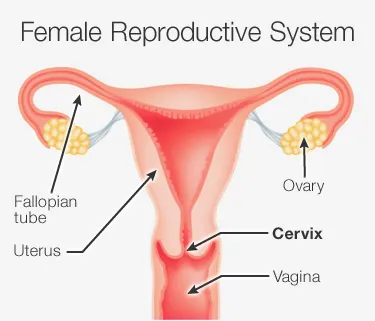
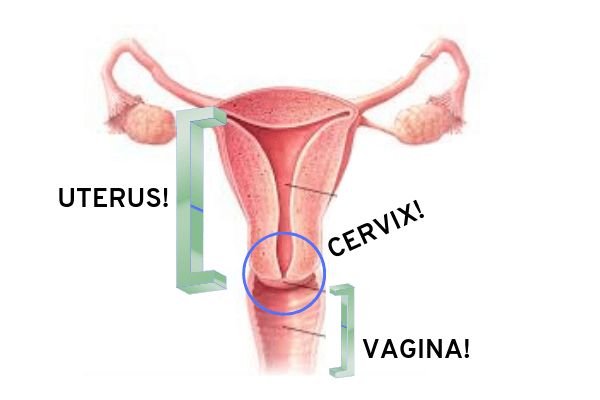
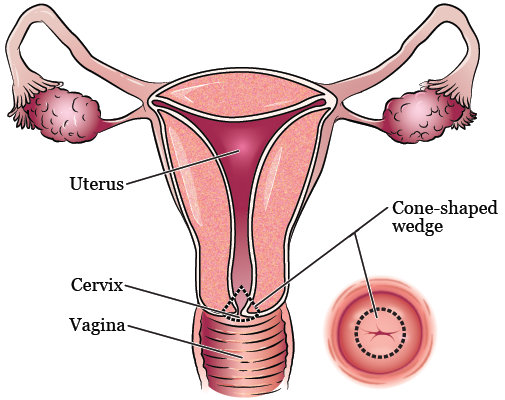
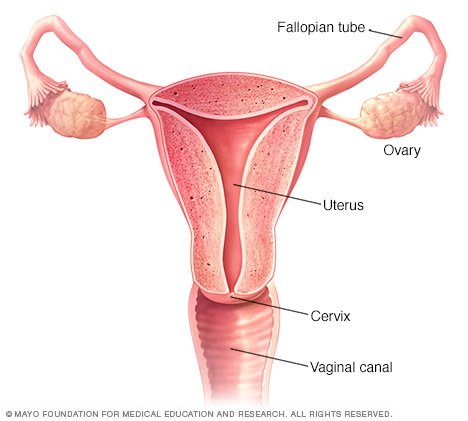
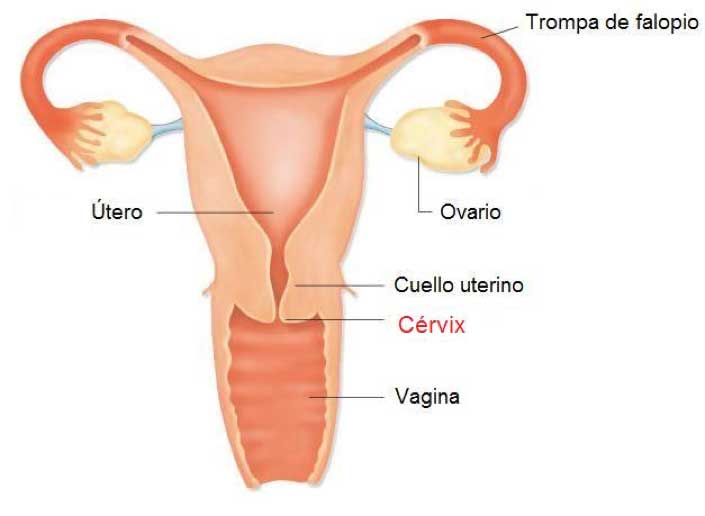
The cervix or cervix uteri (Latin, 'neck of the uterus') is the lower part of the uterus in the human female reproductive system. The cervix is usually 2 to 3 cm long (~1 inch) and roughly cylindrical in shape, which changes during pregnancy. The narrow, central cervical canal runs along its entire length, connecting the uterine cavity and the lumen of the vagina. The opening into the uterus is called the internal os, and the opening into the vagina is called the external os. The lower part of the cervix, known as the vaginal portion of the cervix (or ectocervix), bulges into the top of the vagina. The cervix has been documented anatomically since at least the time of Hippocrates, over 2,000 years ago.
The human female reproductive system. The cervix is the lower narrower portion of the uterus.
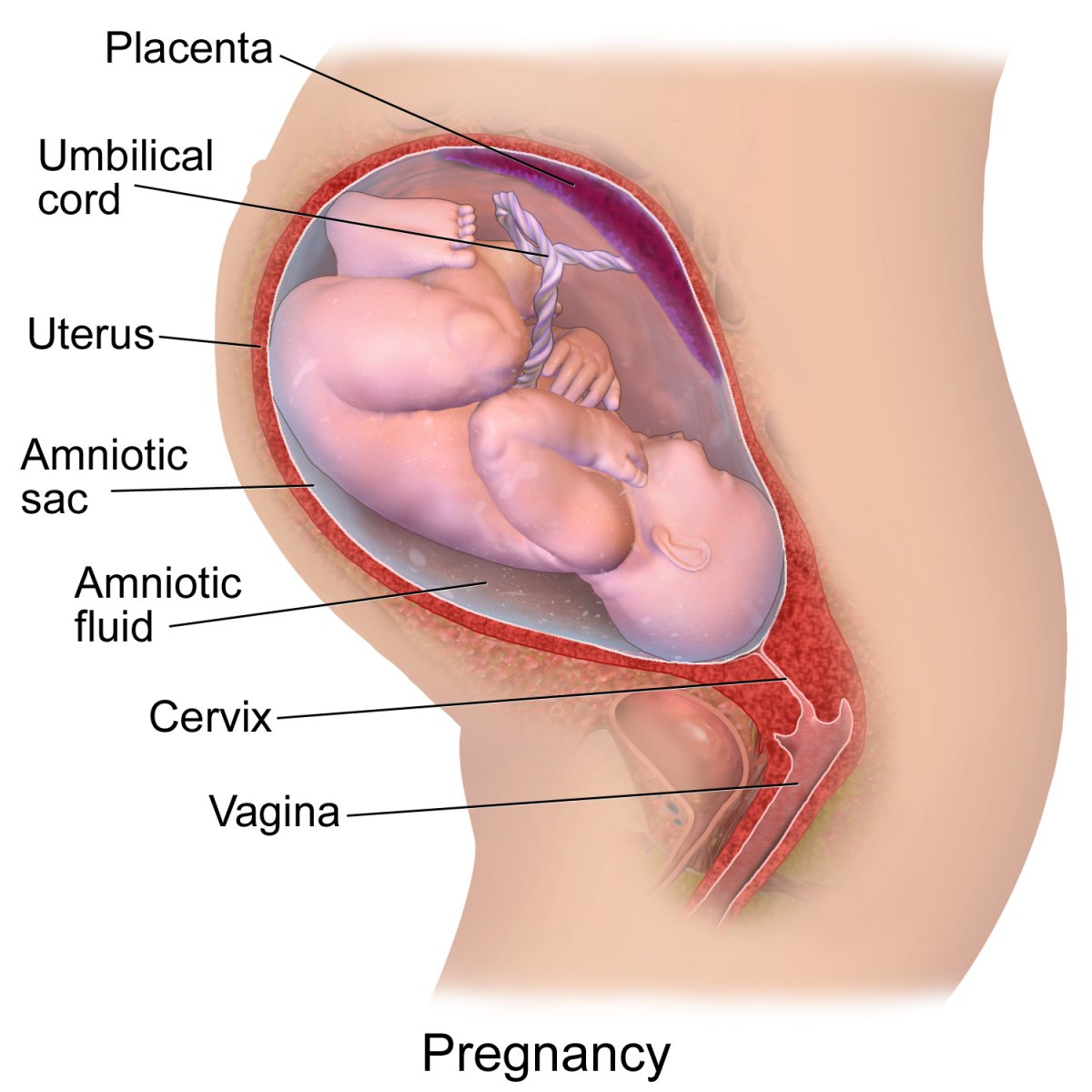
The cervical canal is a passage through which sperm must travel to fertilize an egg cell after sexual intercourse. Several methods of contraception, including cervical caps and cervical diaphragms, aim to block or prevent the passage of sperm through the cervical canal. Cervical mucus is used in several methods of fertility awareness, such as the Creighton model and Billings method, due to its changes in consistency throughout the menstrual period. During vaginal childbirth, the cervix must flatten and dilate to allow the fetus to progress along the birth canal. Midwives and doctors use the extent of the dilation of the cervix to assist decision-making during childbirth.
The cervical canal is lined with a single layer of column-shaped cells, while the ectocervix is covered with multiple layers of cells topped with flat cells. The two types of epithelia meet at the squamocolumnar junction. Infection with the human papillomavirus (HPV) can cause changes in the epithelium, which can lead to cancer of the cervix. Cervical cytology tests can often detect cervical cancer and its precursors, and enable early successful treatment. Ways to avoid HPV include avoiding sex, using condoms, and HPV vaccination. HPV vaccines, developed in the early 21st century, reduce the risk of cervical cancer by preventing infections from the main cancer-causing strains of HPV.[1]
The cervix is part of the female reproductive system. Around 2–3 centimetres (0.8–1.2 in) in length,[2] it is the lower narrower part of the uterus continuous above with the broader upper part—or body—of the uterus.[3] The lower end of the cervix bulges through the anterior wall of the vagina, and is referred to as the vaginal portion of cervix (or ectocervix) while the rest of the cervix above the vagina is called the supravaginal portion of cervix.[3] A central canal, known as the cervical canal, runs along its length and connects the cavity of the body of the uterus with the lumen of the vagina.[3] The openings are known as the internal os and external orifice of the uterus (or external os) respectively.[3] The mucosa lining the cervical canal is known as the endocervix,[4] and the mucosa covering the ectocervix is known as the exocervix.[5] The cervix has an inner mucosal layer, a thick layer of smooth muscle, and posteriorly the supravaginal portion has a serosal covering consisting of connective tissue and overlying peritoneum.[3]
In front of the upper part of the cervix lies the bladder, separated from it by cellular connective tissue known as parametrium, which also extends over the sides of the cervix.[3] To the rear, the supravaginal cervix is covered by peritoneum, which runs onto the back of the vaginal wall and then turns upwards and onto the rectum, forming the recto-uterine pouch.[3] The cervix is more tightly connected to surrounding structures than the rest of the uterus.[6]
The cervical canal varies greatly in length and width between women or over the course of a woman's life,[2] and it can measure 8 mm (0.3 inch) at its widest diameter in premenopausal adults.[7] It is wider in the middle and narrower at each end. The anterior and posterior walls of the canal each have a vertical fold, from which ridges run diagonally upwards and laterally. These are known as palmate folds, due to their resemblance to a palm leaf. The anterior and posterior ridges are arranged in such a way that they interlock with each other and close the canal. They are often effaced after pregnancy.[6]
The ectocervix (also known as the vaginal portion of the cervix) has a convex, elliptical shape and projects into the cervix between the anterior and posterior vaginal fornices. On the rounded part of the ectocervix is a small, depressed external opening, connecting the cervix with the vagina. The size and shape of the ectocervix and the external opening (external os) can vary according to age, hormonal state, and whether natural or normal childbirth has taken
Like Handjob
Bbw Fuck Shower
French Temptress Porn
Pretty Girl Pictures
Little Porn Nude
Cervix (Human Anatomy): Diagram, Location, Conditions ...
Cervix - Wikipedia
Female Genital System Part I: Vulva, Vagina, and Cervix
The Cervix: What it is, and how to find (and feel) it
How to Feel Your Cervix: 9 Steps (with Pictures) - wikiHow
Cervix Penetration: 10 Things You Need to Know
Vagina - Wikipedia
Vagina Cervix


















%3amax_bytes(150000)%3astrip_icc()/what-does-a-fertile-cervix-look-and-feel-like-1960297-v1-51d897046f3245258a2fb8d53357f145.png)










%3amax_bytes(150000)%3astrip_icc()/female-cervix--illustration-651425465-5bf3fe86c9e77c0027fd4e2c.jpg)