Viral load and the PCR
reblogged by Corona InvestigativeWhy they cant be used to prove HIV infection
by Christine Johnson
“Biotechnology’s version of the Xerox machine”— that’s what Forbes magazine called the polymerase chain reaction (PCR). This revolutionary technique enables a scientist to take a sample containing a minute amount of DNA and replicate that DNA sequence until there are a million copies instead of just one or two. Kary Mullis, inventor of PCR, won a 1993 Nobel prize for his billion-dollar invention, which has become indispensable to any genetics lab. It is ironic that one of the first applications of PCR was to detect HIV, considering that Mullis himself doesn’t believe his invention is capable of this. Mullis states the problem is PCR is too efficient – it will amplify whatever DNA is in the sample, regardless of whether that DNA belongs to HIV or a contaminant. And how do you decide which part of the amplified material could be HIV and which part the contaminant(s), if you couldn’t detect HIV in the sample without using PCR? One of the main arguments against the HIV/AIDS hypothesis is that, when employing traditional methods of virus detection, HIV has never been inferred in significant amounts in people with AIDS. Virus culture, for instance, has been adequate to find other viruses, but not HIV. Why not? When virus culture is employed to detect HIV, HIV is never seen or even looked for in the cultures. Its presence is measured by very indirect methods: assays for detection of reverse transcriptase or a p24 protein, neither of which is specific for HIV. Indirect methods would not be necessary if a significant amount of HIV were there to begin with. In other words, if a meaningful amount of HIV were present, the time-honoured laboratory techniques should be able to find it. They can’t. Now we need not only PCR, but continuous modifications and improvements on PCR, in order to try to find HIV. This is how the idea of “viral load” came about, inspired by two spates of scientific papers that claimed HIV is busily replicating by the billions: initially, papers claiming HIV was “hiding in the lymph nodes,”1,2 and more recently, the Ho and Wei papers.3,4 The latter studies attempted to measure “viral load” at a given point, after which “antiviral” drugs were administered to the patient. The drugs were supposed to prevent replication of any new HIV, and the viral load would decrease accordingly. However, within a few days, the remaining virus would mutate into a form resistant to the drugs, and in a few weeks the viral load would return to its pre-treatment levels. Applying a mathematical formula to this dynamic, the rate at which the virus replicates was allegedly determined. Hence was born what I call “Dr. Ho’s kitchen sink theory”. According to Ho, billions of copies of HIV are being made every day, which infect billions of T4-cells. These T-cells are destroyed not by HIV, but by the immune system. They are replenished every day, but over the years, the immune system loses ground and HIV finally wins. This process was likened to a sink with the drain open, the water pouring in from a tap (new T-cells being made) at a slightly lower rate than it drained away (infected T-cells being destroyed). It is most important to note that the viral load studies all rely completely on PCR and related techniques. This article will discredit PCR as an accurate method of determining HIV infection, which will in turn cast doubt on any conclusions about HIV that have been made based on PCR techniques.

How PCR works
The theory of HIV says it, like other suggested retroviruses, contains RNA but no DNA: when HIV is said to infect a cell, the reverse transcriptase enzyme is thought to transform the RNA into complementary DNA, which is then inserted into the host cell’s DNA. Therefore, if PCR is used to analyse human tissue for the presence of HIV, it would be looking for only a short segment out of the entire cellular DNA strand. This short segment represents the genetic material proposed for HIV, that in theory has been incorporated into the DNA of the cell. (Viral load studies try to look for cell-free HIV. Even here, PCR is only looking for part of HlV’s entire proposed genetic package, or genome, not an entire virus.)
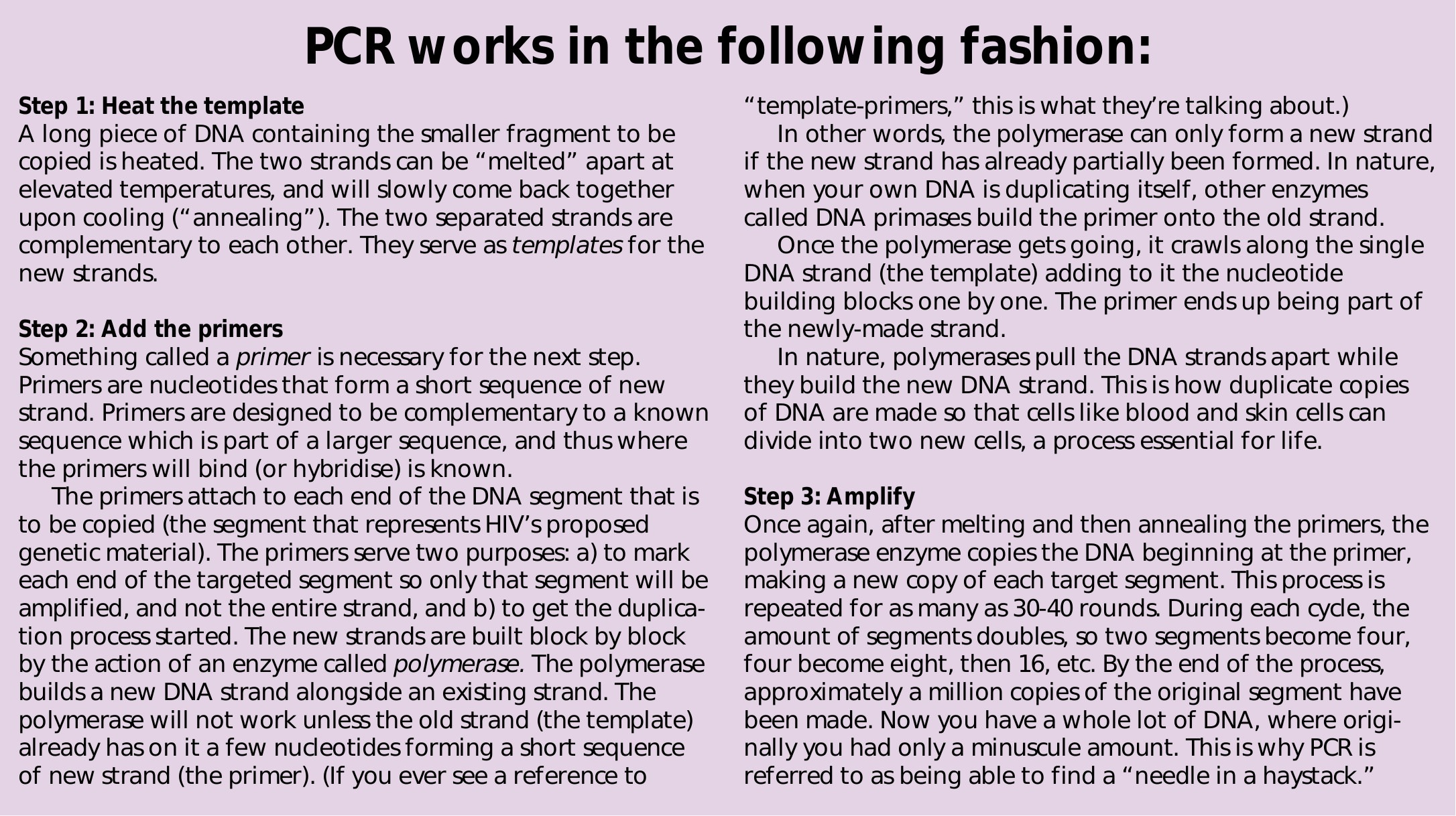
Obviously, it is necessary for the primers to be specific to HIV. Whether the PCR will make an amplified product (a “positive PCR”) depends on whether the primers you add match part of the DNA in the target specimen. Below, we will see that the specificity of the primers for HIV is in doubt. Even if the primers were specific to HIV, if similar sequences are present in the target, the primers, under lax conditions, will form hybrids with (or bind) related sequences that are less than a perfect match. They will then prime the polymerase, which starts the amplification procedure, even though no HIV was present to begin with.
USING PCR TO FIND HIV
A problem for the HIV hypothesis was that, even with the use of standard PCR, researchers could not find much, if any, HIV in persons with AIDS diagnoses. To resolve this paradox, the authors of the new “viral load” papers came up with two modifications of PCR, which they claimed were much more efficient at finding HIV. These were the QCPCR and the branched DNA test (bDNA). And suddenly – eureka! – billions of copies of what was believed to be HIV were found. The contradiction here seems to have escaped the authors of these papers: Why would such powerful new tests be needed at all to find a microbe that is present in the billions? Traditional methods should suffice.
QC-PCR
This is the test used in the above-mentioned papers by Anthony Fauci (Pantaleo) and Ashley Haase (Embretson), which claimed HIV was “hiding in the Iymph nodes.” These papers were accepted as fact, even though QC-PCR was, and remains, an unvalidated technique. Mark Craddock, of the University of Sydney (Australia), explained the principles of and problems with QC-PCR as follows:8 “PCR mass produces fragments of DNA. You start with a small amount of DNA and after each PCR cycle, the amount of DNA you have is between one and two times the amount at the beginning of the cycle. Thus, the amount of DNA you have to study increases exponentially. The fact that the PCR is an exponential growth process means that experimental errors will also grow exponentially, so you need to be very careful about what you do with the process. “A number of people have decided that it should be possible to estimate the amount of DNA present in a sample by using PCR. This is the so-called quantitative competitive PCR. The idea is to add to the sample to be estimated a known amount of similar but distinguishable DNA and amplify both together. The assumption is that the relative amounts of the two products should stay the same, and hence you can work out the size of the sample you started with by knowing the ratio of the two, determined by observation when PCR has produced enough of both to measure, and how much control DNA was added. “What is absolutely crucial is that the relative amounts of the test DNA and your known control must remain exactly equal. Close is not good enough. The slightest variations will be magnified exponentially and can produce massive errors in your estimate. “The difficulties in using PCR quantitatively were pointed out by Luc Raeymaekers in the journal Analytical Biochemistry in 1993. He noted published papers on QC-PCR contain data that show that the fundamental assumption that the relative sizes of the samples remain constant is not met in practice. Despite this, HIV researchers continue to use PCR to quantify viral load. There is simply no way of knowing whether a given estimate is correct or is 100,000 times too high!” Todd Miller calls QC-PCR the “latest fad in science” and agrees that if the relative amounts of your test DNA and your known control are not equal, there is one thing you can say for sure about the estimate of your starting target (the amount of proposed HIV RNA in the patient’s blood sample): It will be wrong. How did QC-PCR, with all its flaws, become an acceptable HIV test? Miller explains: “The way this situation has manifested itself in modern science is like this: First some people spend a lot of time trying to get this test to work, and if they’re lucky, end up publishing papers about caveats in the procedure. Second, others happen to get the test to give them an answer that “makes sense” and publish their data as a significant contribution to the field. Third, because of its relative newness and arcane nature, it remains as quasi-accepted with many passive sceptics and a few users. However, most who use it are more interested in their own pet phenomenon than in the mechanics of the reaction.”
bDNA BRANCHED DNA PCR
This is the test used in Ho’s paper. Though it is not, strictly speaking, PCR, it is referred to as such since it incorporates PCRtype technology. The difference is that bDNA amplifies the signal, not the target. That is, regular PCR makes more of the target so you can find it, whereas bDNA sort of shines a bright spotlight on it so you can see it better. Project Inform was kind enough to send me the following explanation of how bDNA works:9 “Copies of a DNA probe are attached to the wall of a small laboratory vessel; then the sample is put in. [A DNA probe is a small piece of DNA complementary to the target DNA sequence.] This probe binds to a certain part of HIV RNA, if it is found in the sample, holding the RNA in the vessel. Then another DNA probe is put in; one end of this attaches to another part of the HIV RNA. The other end of the second probe has many branches and each branch ends with a “reporter” chemical that, under certain conditions, will produce light, which can be detected by laboratory equipment. Each molecule of HIV RNA can attach to one of these branching structures and hold on to a small number of light sources, not just one. In this way, very small amounts of the target RNA can be detected, without the need for PCR amplification.” In his initial paper, Ho gave no data on the protocols for this test or whether it was reliable. The reader was referred to two other papers that were “in press”. So, no data was available at that time to anyone who wanted to verify this method. The data obtained from bDNA was confirmed by QC-PCR, the details of QC-PCR being set out in a reference authored by four coauthors of the Wei study, hardly what you might call independent or objective researchers. In the tradition of HIV research, unproven theories and faulty studies are accepted without question and incorporated into the “conventional wisdom” before being properly validated. By then, the damage is done, and if subsequent flaws are discovered it hardly matters. The mechanics of bDNA are complex: Five different hybridisation reactions are going on. Hybridisation is a standard technique wherein a DNA probe is put into a sample and will bind to any complementary segments it finds. It’s another indirect test, and it has a lot of problems. According to molecular biologist Bryan Ellison, “The only time molecular biology works is if you purify things first. There’s always the possibility of cross-reactions, especially when you put your probes into a big soup of proteins” (which is exactly what the target blood sample is). Duesberg pointed out the following: After making the appropriate adjustments to his calculations, Ho himself later found that more than 10,000 viruses inferred by the bDNA assay used in his Nature paper would actually correspond to less than one infectious virus, leading one to wonder what it is that is actually being measured on these tests.10 Yet these speculative and unvalidated papers have been accepted as gospel truth! In Ellison’s mind, Ho’s study is “Pure fantasy. There’s never been a paper that shows viral load.”
The Problems with PCR
THE ACCURACY OF PCR HAS NEVER BEEN VERIFIED BY A PROPER GOLD STANDARD To find out if any diagnostic test for HIV infection actually works, it is necessary to verify the test with an independent gold standard. The only proper gold standard for this purpose is HIV itself. In other words, the results of your experimental test, whether it’s PCR or anything else, must be compared to the results of virus isolation in each sample tested. If virus is actually found in each patient with a positive PCR, and no virus is found in each patient with a negative PCR, then you could say PCR is extremely accurate for detecting HIV. The concept of virus isolation as a gold standard is particularly important in the case of HIV, since HIV has been extremely difficult, if not impossible, to define in genetic or molecular terms. Even if anyone had ever accomplished virus isolation for HIV11, it has never been used as a gold standard for any HIV diagnostic test, including PCR. As it stands right now, bDNA uses QC-PCR as a gold standard; QC-PCR uses regular PCR as a gold standard; regular PCR uses antibody tests as a gold standard, and antibody tests use each other. I have noticed time after time that studies which are “verifying” an HIV antibody test will invariably state that they evaluated the performance of their test on samples which were known to be TRUE-POSITIVE or TRUE-NEGATIVE. How did they know this? It’s simple: Without a gold standard, they didn’t. It is sometimes argued that “studies have shown” these tests to agree with each other or confirm each other’s findings, and therefore they must be correct. This is not rigorous scientific thinking. Sometimes you can get the results of different tests to agree with each other, but that does not prove anything – no more than it would prove if five criminals all agreed that they were somewhere else when the bank was being robbed. Eleopulos says the following about the importance of gold standards: “The use of viral isolation as an independent means of establishing the presence or absence of the virus is technically known as a gold standard, and is a quintessential element for the authentication of any diagnostic test. Without a gold standard, the investigator is hopelessly disoriented, since he does not have an autonomous yardstick against which he can appraise the test he is aspiring to develop.... Only by this means can we assure patients that a positive HIV PCR is only ever found in the presence of HIV infection, that is, the tests are highly specific for HIV infection.“ Even well-known AIDS researcher William Blattner has conceded that “one difficulty in assaying the specificity and sensitivity of human retrovirus assays (including HIV) is the absence of a final ‘gold standard.’ In the absence of gold standards for both HTLV-1 and HIV-1, the true sensitivity and specificity for the detection of viral antibodies remain imprecise.”12 Mark Craddock states QC-PCR is unverified and probably unverifiable. He asks, “If PCR is the only way that the virus can be detected, then how do you establish the precise viral load independently of PCR, so that you can be certain that the figures PCR gives are correct?” All this has apparently been lost on AIDS researchers, as it is regularly recommended that PCR, particularly QC-PCR, be used as a gold standard for other HIV tests.9,13
THE SPECIFICITY OF PCR HAS NEVER BEEN DETERMINED Specificity means how often a test will give negative results in people who are not infected. A test’s specificity rating reveals the level of false-positive results to expect when using that test. Without a virus isolation gold standard, the true specificity will never be known. Even using concordance with antibody tests as a gold standard, PCR was not found to be very specific for HIV.6 Citing a proficiency study involving five laboratories with extensive PCR experience, Sloand states that the average specificity was 94.7%.14 Specificity was as low as 90%. Numbers in the 90s may sound good, but in reality, this is not the case. The number of falsepositives compared to true positives is dependent on the prevalence of HIV infection in any population being tested15 – the lower the prevalence, the more false-positives. Sloand comments that if the specificity levels achieved in this study were applied to the potential blood donor population” (blood donors now consisting of members of the low-prevalence general population), then “...for every true silent infection detected, 1800 uninfected donors would be classified as PCR positive and 3500 as PCR indeterminate. Thus PCR is clearly not suitable for routine screening of transfused blood” and by inference, any low-prevalence population. At a specificity of 90%, I would say it wasn’t suitable for testing any population. In a FAX I received from the Centers for Disease Control (CDC) in 1994 regarding PCR, they stated that “Neither its specificity nor its sensitivity is known,” and that “PCR is not recommended and is not licensed for routine diagnostic purposes.”16 In a nutshell, “The specificity of any form of PCR, for the HIV genome, has not been determined.”5
PCR PRIMERS ARE NOT SPECIFIC According to Eleopulos, Turner, and Papadimitriou, “The minimum requirement for [interpreting that a positive PCR signal, or hybridisation in general, proves HIV infection] is prior proof that the PCR primers and the hybridisation probes belong to a unique retrovirus, HIV, and that the PCR and hybridisation reactions are HIVspecific.” Turner told me: “The PCR genomic arguments require isolation of HIV as absolutely essential. Otherwise how does anyone know the origin of the nucleic acid?” Eleopulos disputes the reality of a distinct HIV genome. Conceding its existence for the sake of argument, she offers the following evidence to demonstrate PCR is nonspecific for HIV:17
- There is no way to be sure the “HIV” nucleic acid probes and PCR primers are specific to HIV because: most, if not all, probes used for hybridisation assays, including the PCR probes and primers, are obtained from “HIV” grown in tissue cultures using cells (called a cell line) taken from a patient with T4 cell leukemia, a disease which Gallo claims is caused by a retrovirus similar to HIV – HTLV-I. And recently a retrovirus is claimed to have been isolated from a non-HIV-infected cell culture using another cell line. Thus the standard cell lines used to grow HIV have been shown to indicate other retroviruses. Since even the well-established method for isolating retroviruses (which to date has never been done for HIV) cannot distinguish one retrovirus from another, one cannot be confident that “HIV” nucleic acid probes and PCR primers are indeed specific for HIV.
- Proposed HIV genes hybridise with the structural genes of HTLV-I and HTLV-II, two other human retroviruses. This means that if the probes find genetic material from these other retroviruses, they will stick to it and give a signal that they have found HIV instead. Since it is accepted that 10% of AIDS-diagnosed patients carry HTLV-I and that the normal human genome contains sequences related to HTLV-I and HTLV-II, this type of cross-reaction can be anticipated.
- Normal human cells contain hundreds or thousands of retrovirus-like sequences, that is, small stretches of DNA that match a small part of the proposed genome of HIV or other retroviruses. And, since PCR often amplifies just a small part of the entire genome of whatever it’s looking for, how do you know that what it finds isn’t a normal cellular gene sequence that just happens to match part of what’s proposed for HIV?
- Further evidence that PCR is nonspecific is that positive PCRs can be obtained from cells without nucleic acids. So if there’s no nucleic acid, there’s no DNA or RNA, and if there’s no DNA or RNA, there’s certainly no HIV
- The chemicals used in labs in the preparation of tissue cultures (called buffers and reagents) may give positive PCR signals for HIV.18
PCR DETECTS ONLY A SMALL FRAGMENT OF AN ENTIRE VIRUS PCR detects at best single genes and most often, only bits of genes. If PCR finds two or three genetic fragments out of a possible dozen complete genes, this is not proof that all the genes (the entire genome) are present. Part of a gene does not equal a complete virus particle. HIV experts admit that the majority of proposed HIV genomes are incomplete; they could never orchestrate the synthesis of a virus particle. Turner explains: “Even if all genomes were complete, having the plans doesn’t mean you’ve built the house. You can carry a whole retroviral genome around inside your cells all your life without ever making a virus particle.” These two problems make it even more uncertain what the significance of a positive PCR is.
THE FINDING OF “HIV RNA” ON PCR DOES NOT SIGNIFY THE PRESENCE OF HIV These days, one keeps hearing the phrase “HIV RNA PCR.” What’s the difference between that and regular old DNA PCR? Regular PCR looks for the DNA version of what is often accepted to be the HIV genome; RNA PCR looks for the RNA version, that is, free virus that has not infected a cell. With the new notion that HIV was busily replicating by the billions, it was now thought necessary to find how much free virus there might be at any given time. Free virus would contain only RNA, so if the PCR finds a lot of “HIV RNA,” it is believed billions of copies of free virus are swarming around the patient’s tissues. In other words, if you find RNA, you’ve found HIV as well. Since it’s believed HIV contains two strands of RNA, the suggested formula is: Two RNAs = one virus. In actuality, things are not this simple. In 1993, during the “HIV is hiding in the lymph nodes” phase of the viral load theory, Piatak and colleagues, including Shaw, admitted that in order to determine the quantity of HIV particles, one must have prior evidence that the RNA actually belongs to an HIV particle. 5 No such evidence was presented. No relationship has yet been established between the amount of RNA and the amount of particles that may or may not be present. And no one has established whether the RNA comes from a virus particle or from somewhere else. Without virus isolation, how do you know the origin of the nucleic acid (RNA)?
CELL-FREE VIRUS IS NOT INFECTIOUS VIRUS Even if Ho were right about billions of cell-free HIVs being present in the bloodstream, free virus is by definition not infectious virus; it’s irrelevant as a pathogen. For HIV to infect a cell, its envelope protein, gp120, must bind to the CD4 receptor site on the cell’s surface. However, as far back as 1983, Gallo pointed out that “the viral envelope which is required for infectivity is very fragile. It tends to come off when the virus buds from infected cells, thus rendering the particles incapable of infecting new cells.” Because of this, Gallo said “cell-to-cell contact may be required” for retroviral infection. Since gp120 is “crucial to HlV’s ability to infect new cells,” and since gp120 is not found in the cell-free particles, even if huge amounts of free HIV are present in the blood, they would be non-infectious.17
PCR IS NOT STANDARDISED OR REPRODUCIBLE In a recent paper, Teo and Shaunak commented on in situ PCR: “Despite considerable effort, the technique is still technically difficult and has not yet proved to be reliable or reproducible.”19 In a study which compared PCR results to antibody test results, PCR was found not to be reproducible and “False-positive and falsenegative results were observed in all laboratories (concordance with antibody tests ranged from 40% to 100%).“20
PCR IS SUSCEPTIBLE TO CROSS-CONTAMINATION Minute quantities of nucleic acids from prior specimens can easily contaminate the specimen currently being tested, giving a false-positive result.21 Even microscopic bits of skin or hair from the lab technician can cause this problem. Many sources of cross-contamination exist, and it can occur “at any step in the procedure, from the point of collection of samples through to the final amplification...”22 Other causes of false-positives are enumerated by Teo and Shaunak: “We have now identified a number of factors which can contribute to the poor amplification of the target DNA and to the generation of false-positive signals. These factors include the effects of fixation, reagent abstraction, DNA degradation, DNA end-labelling and product diffusion.... We believe considerable caution should be exercised in the interpretation of results generated using PCR in situ.”19
FALSE-POSITIVES FREQUENTLY OCCUR WITH PCR -
- A proficiency study to rate HIV PCR’s performance on detecting cell-free DNA showed “a disturbingly high rate of nonspecific positivity” using the commonly employed primers (SK38/39, for the gag or p24 gene). In fact, similar rates of positivity were found for both antibody-negative and antibody-positive specimens (18% versus 26%)!23
- Out of 30 uninfected children, 6 had “occasional” positive PCR results.24
- PCR performed on uninfected infants under one year of age showed 9/113 (9 out of 113), 15/143, 13/137, 7/87, and 1/63 infants to have positive PCR tests.25
- Among 117 uninfected children born to HIV-infected mothers, six (5%) had a false-positive PCR on cord blood.26
- In a PCR proficiency study, 54% of the laboratories involved had problems with false-positive results; 9.3% of the total uninfected specimens were reported as positive.22
- One out of 69 antibody-negative, non-seroconverters was PCR positive.2
- A high-risk individual was initially PCR positive but negative on repeat PCR testing of the same specimen by two different laboratories.27
- The World Health Organisation’s PCR working group demonstrated high levels of false-positive results obtained during “blind” HIV PCR studies.22
- Sheppard et al. stated in their study: “This trial demonstrated that false-positive results, even with rigorous testing algorithms, occur with sufficient frequency among uninfected individuals to remain a serious problem.”28
- Out of 327 health care workers exposed by needlestick to HIV, 4 had one or more positive PCR results and 7 had indeterminate results. Later samples for all 11 were negative and none seroconverted or developed p24 antigenemia, leading to the conclusion that “false-positive results occur even under the most stringent test conditions.”29

REFERENCES
1. Embretson J, Zupancicl M, Ribas JL, et al. 1992. “Massive covert infection of helper T lymphocytes and macrophages by HIV during the incubation period of AIDS.” Nature. 362:359-362.
2. Pantaleo G, Graziosi C, Demarest J, et al. 1993. “HIV infection is active and progressive in lymphoid tissue during the clinically latent stage of disease.” Nature. 362:355-358.
3. Ho DD, Neumann AU, Perelson AS, et al. 1995. “Rapid turnover of plasma virions and CD4 lymphocytes in HIV-1 infection.” Nature. 373:123-126.
4. Wei X, Ghosh SK, Taylor ME, et al. 1995. “Viral dynamics in human immunodeficiency virus type 1 infection.” Nature. 373:117-122.
5. Eleopulos E, Turner VF, Papadimitriou J. 1995. “Turnover of HIV-1 and CD4 lymphocytes.” Reappraising AIDS. 3(6):2-4.
6. Eleopulos E, Turner VF, Papadimitriou J. Letter to Nature. 1994. “Is HIV really hiding in the Iymph nodes?”
7. Duesberg P, Bialy H. “Responding to ‘Duesberg and the new view of HIV”’ in AIDS: Virus- or DrugInduced. Kluwer Academic Publishers, Boston (1996).
8. Craddock M. 1995. “HIV: Science by Press Conference.” Reappraising AIDS. 3(5):-4.
9. Project Inform Fact Sheet: PCR Tests. August 1, 1995.
10. Duesberg P, Bialy H. 1995. “HIV an illusion.” Nature. 375:197.
11. Papadopulos-Eleopulos E, Turner VF and Papadimitriou JM. 1993. “Is a positive Western Blot proof of HIV infection?” Bio/Technology. 11:696-707.
12. Blattner WA. 1989. Retroviruses. pp545-592. In Viral Infections in Humans, third edition, edited by A Evans. Plenum Medical Book Company, New York.
13. Macy E, Adelman D. 1988. Letter to New England Journal of Medicine. December 15.
14. Sloand E, Pitt E, Chiarello R, et al. 1991. “HIV Testing: State of the art.” JAMA. 266:2861.
15. Maver, Robert. April 1993. “Testing AIDS Tests.” Rethinking AIDS. 1(4):4.
16. Centers for Disease Control Faxback document #320320, January 1993.
17. Eleopulos E, Turner VF, Papadimitriou J, Causer D. 1995. “Factor Vlll, HIV, and AIDS in hemophiliacs: An analysis of their relationship.” Genetica. 95(1-3):25-50.
18. Conway B. 1990. “Detection of HIV-1 by PCR in Clinical Specimens,” p40-45, in Techniques in HIV Research, edited by A Aldovini and BD Walker, MacMillan, New York.
19. Teo IA, Shaunak S. 1995. “PCR in situ: aspects which reduce amplification and generate falsepositive results.” Histochem. J. 27:660.
20. Defer C, Agut H, Garbarg-Chenon A, et al. 1992. “Multicentre quality control of polymerase chain reaction for detection of HIV DNA.” AIDS. 6:659.
21. Bootman JS, Kitchin PA. 1994. “Reference preparations in the standardization of HIV-1 PCR: An international collaborative study.” J. Vir. Meth. 49:1-8.
22. Bootman JS, Kitchin PA. 1992. “An international collaborative study to assess a set of reference reagents for HIV-1 PCR.” J. Vir. Meth. 37:23.
23. Busch MP, Henrard DR, Hewlett IK, et al. 1992. “Poor sensitivity, specificity, and reproducibility of detection of HIV-1 DNA in serum by polymerase chain reaction.” J. AIDS. 5:872.
24. Garbarg-Chenon A, Segondy M, Conge A, et al. 1993. “Virus isolation, polymerase chain reaction and in vitro antibody production for the diagnosis of pediatric human immunodeficiency virus infection.” J. Vir. Methods. 42:117.
25. Paui MO, Tetali S, Lesser ML, et al. 1996. “Laboratory diagnosis of infection status in infants perinatally exposed to human immunodeficiency virus type 1.” J. Inf. Dis. 173:68.
26. Simonon A, Lepage P, Karita E, et al. 1994. “An assessment of the timing of mother-to-child transmission of human immunodeficiency virus type 1 by means of polymerase chain reaction.” J. AIDS. 7:952.
27. Celum CL, Coombs RW, Lafferty W, et al. 1991. “Indeterminate human immunodeficiency virus type 1 Western Blots: Seroconversion risk, specificity of supplemental tests, and an algorithm for evaluation.” J. Inf. Dis. 164:656.
28. Sheppard HW, Ascher MS, Busch MP, et al. 1991. “A multicenter proficiency trial of gene amplification (PCR) for the detection of HIV-1.” J. AIDS. 4:277.
29. Gerberding JL. 1994. “Incidence and prevalence of human immunodeficiency virus, hepatitis B virus, hepatitis C virus, and cytomegalovirus among health care personnel at risk for blood exposure: Final report from a longitudinal study.” J. Inf. Dis. 170:1410.
Reblogged from: Continuum Vol. 4, No. 4, Nov/Dec. 1996, pp. 32 - 37