Uterus Prolapse

🛑 ALL INFORMATION CLICK HERE 👈🏻👈🏻👈🏻
Uterus Prolapse
Written by Lori Smith, BSN, MSN, CRNP on November 22, 2017
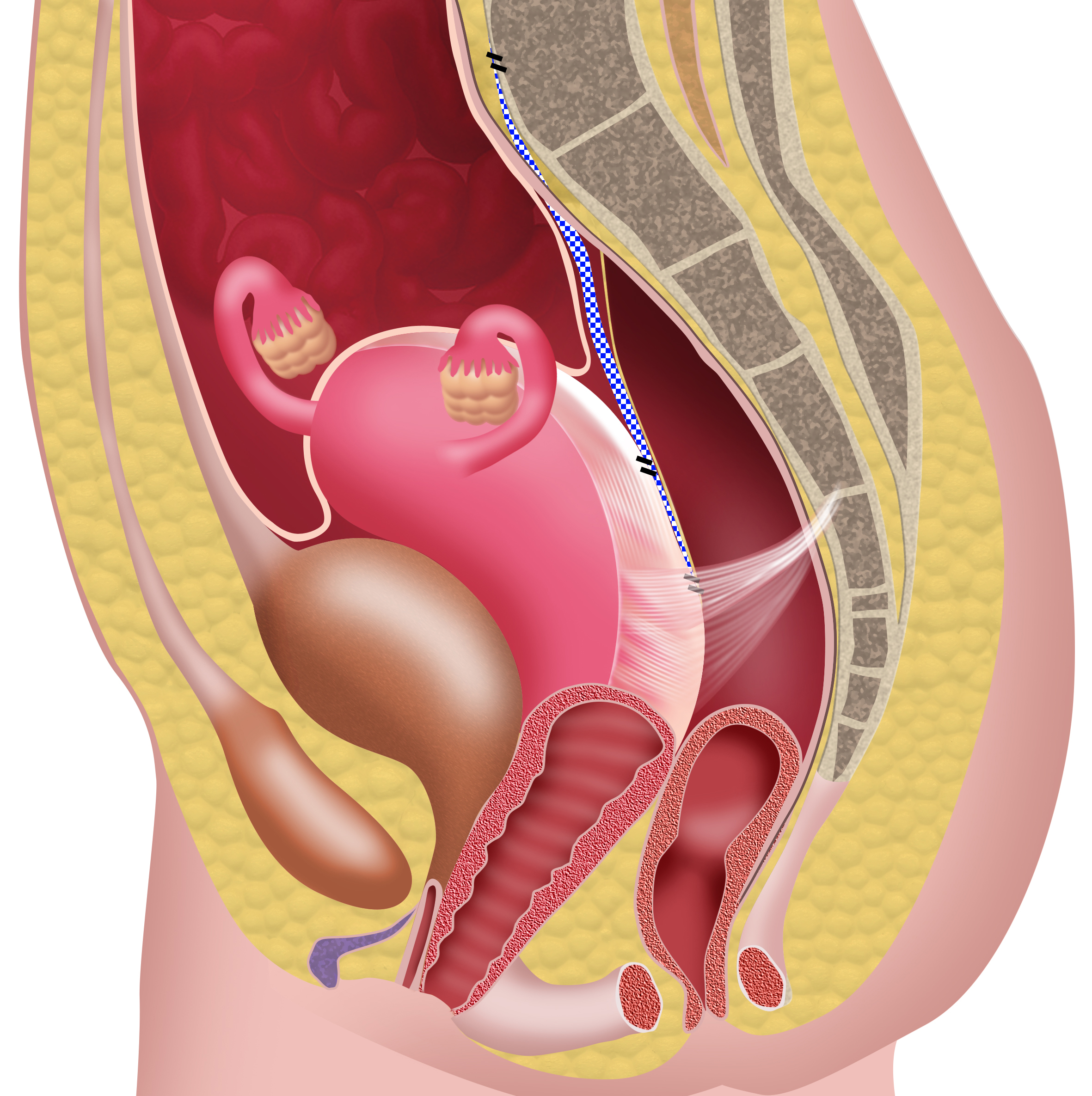
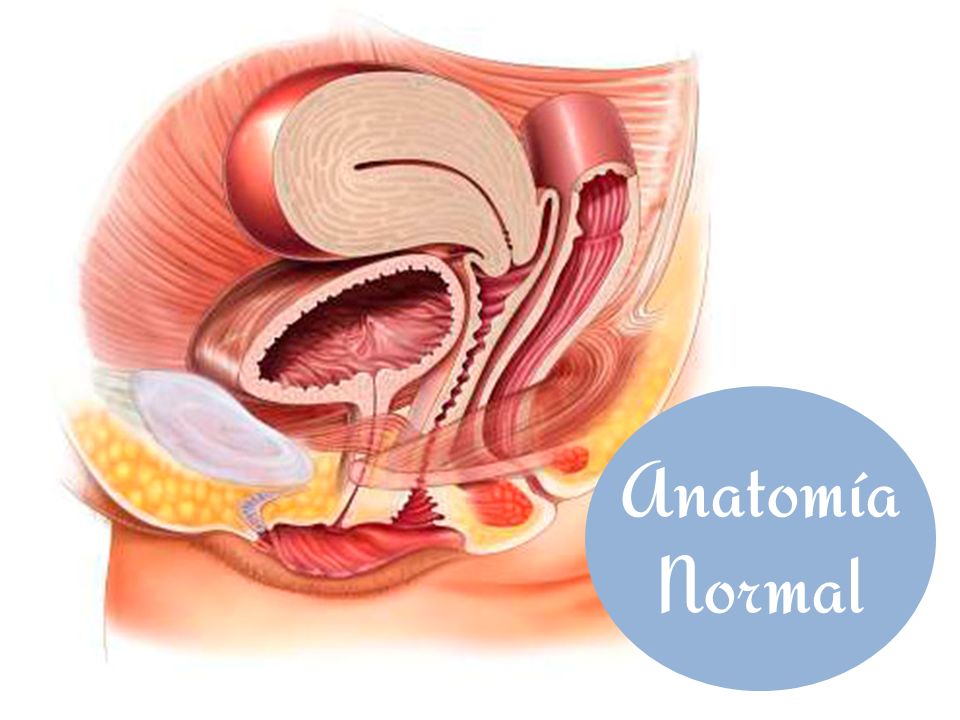
Share on Pinterest The uterus, also known as the womb, is held above the vagina by the pelvic floor muscles and ligaments.
Written by Lori Smith, BSN, MSN, CRNP on November 22, 2017
Medically reviewed by Jillian Kubala, MS, RD
© 2004-2021 Healthline Media UK Ltd, Brighton, UK, a Red Ventures Company. All rights reserved. MNT is the registered trade mark of Healthline Media. Any medical information published on this website is not intended as a substitute for informed medical advice and you should not take any action before consulting with a healthcare professional
© 2004-2021 Healthline Media UK Ltd, Brighton, UK, a Red Ventures Company. All rights reserved. MNT is the registered trade mark of Healthline Media. Any medical information published on this website is not intended as a substitute for informed medical advice and you should not take any action before consulting with a healthcare professional
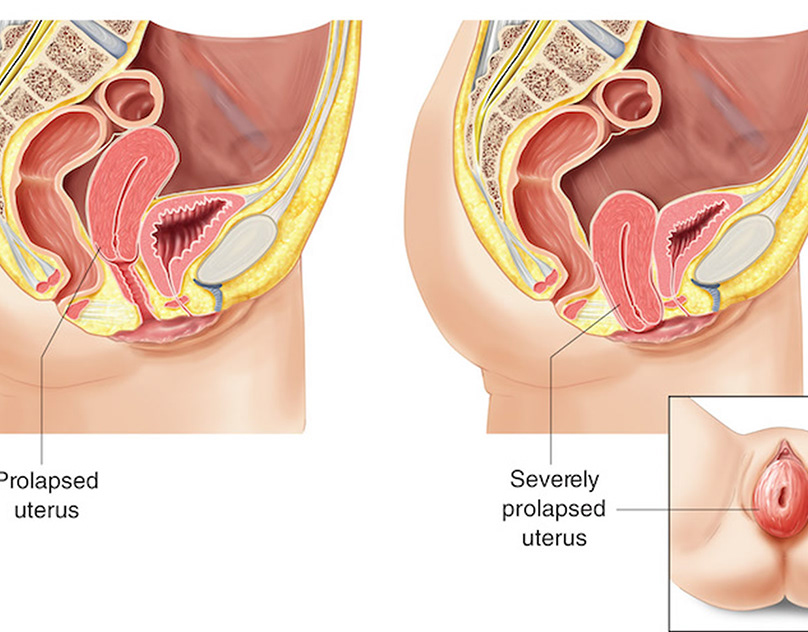
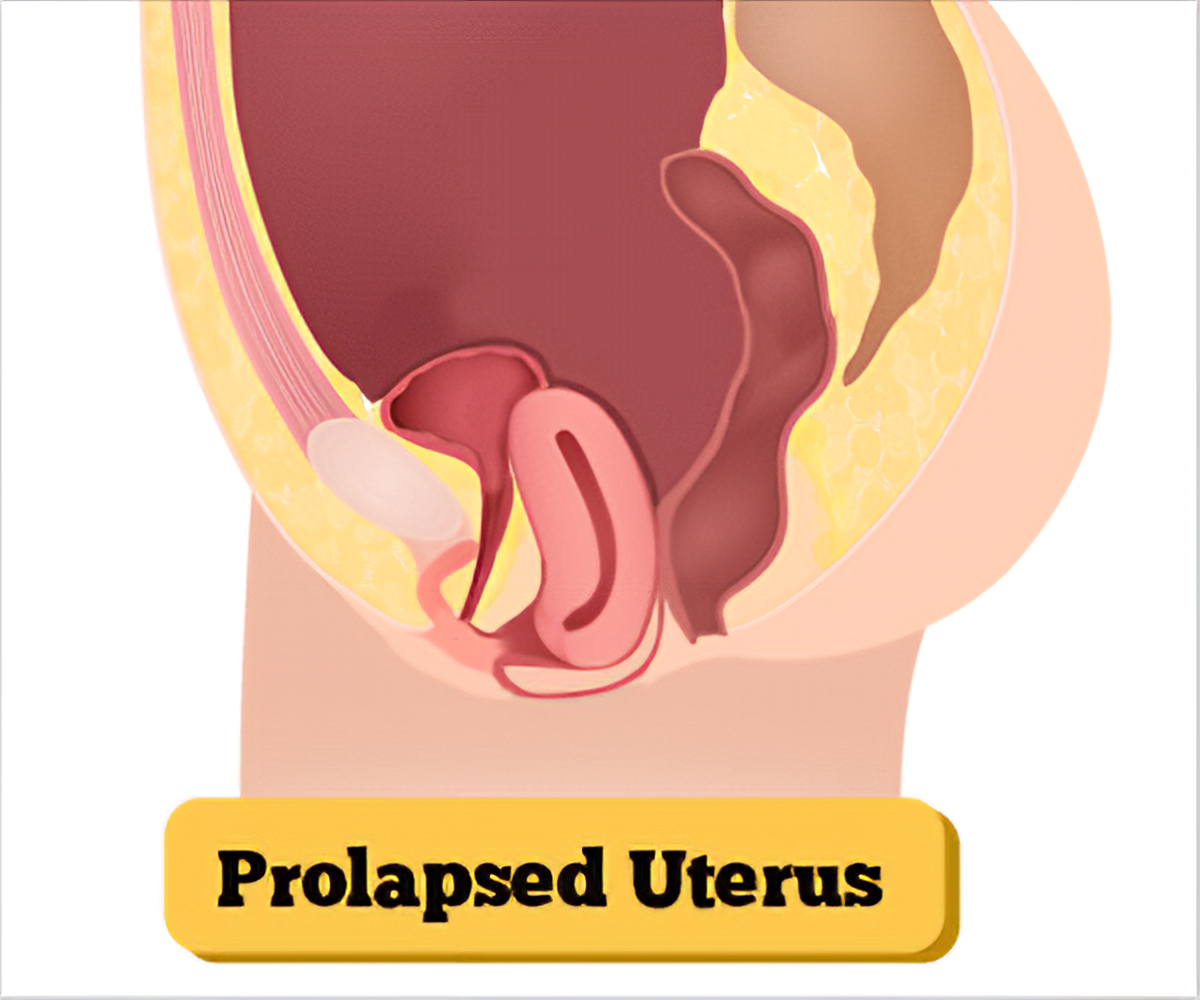
A uterine prolapse is when the uterus descends toward or into the vagina. It happens when the pelvic floor muscles and ligaments become weak and are no longer able to support the uterus.
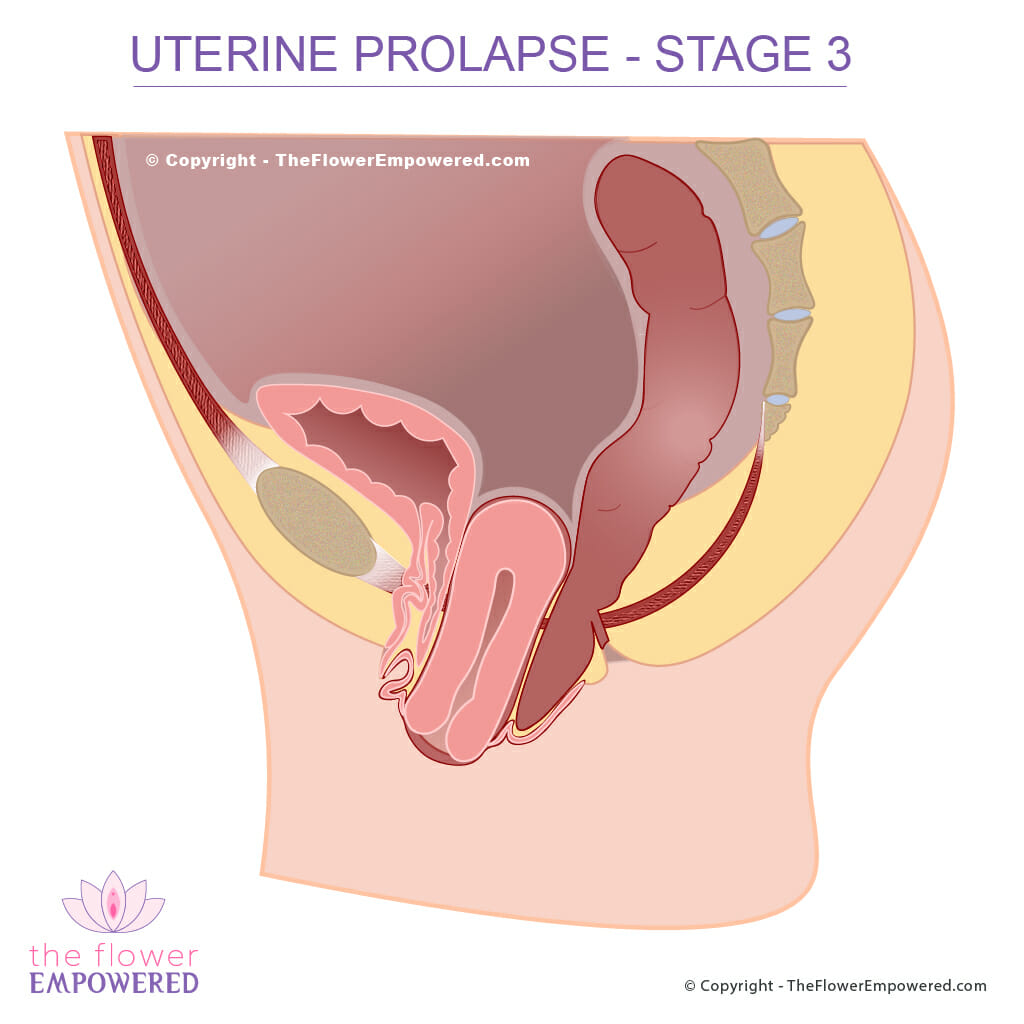
In some cases, the uterus can protrude from the vaginal opening.
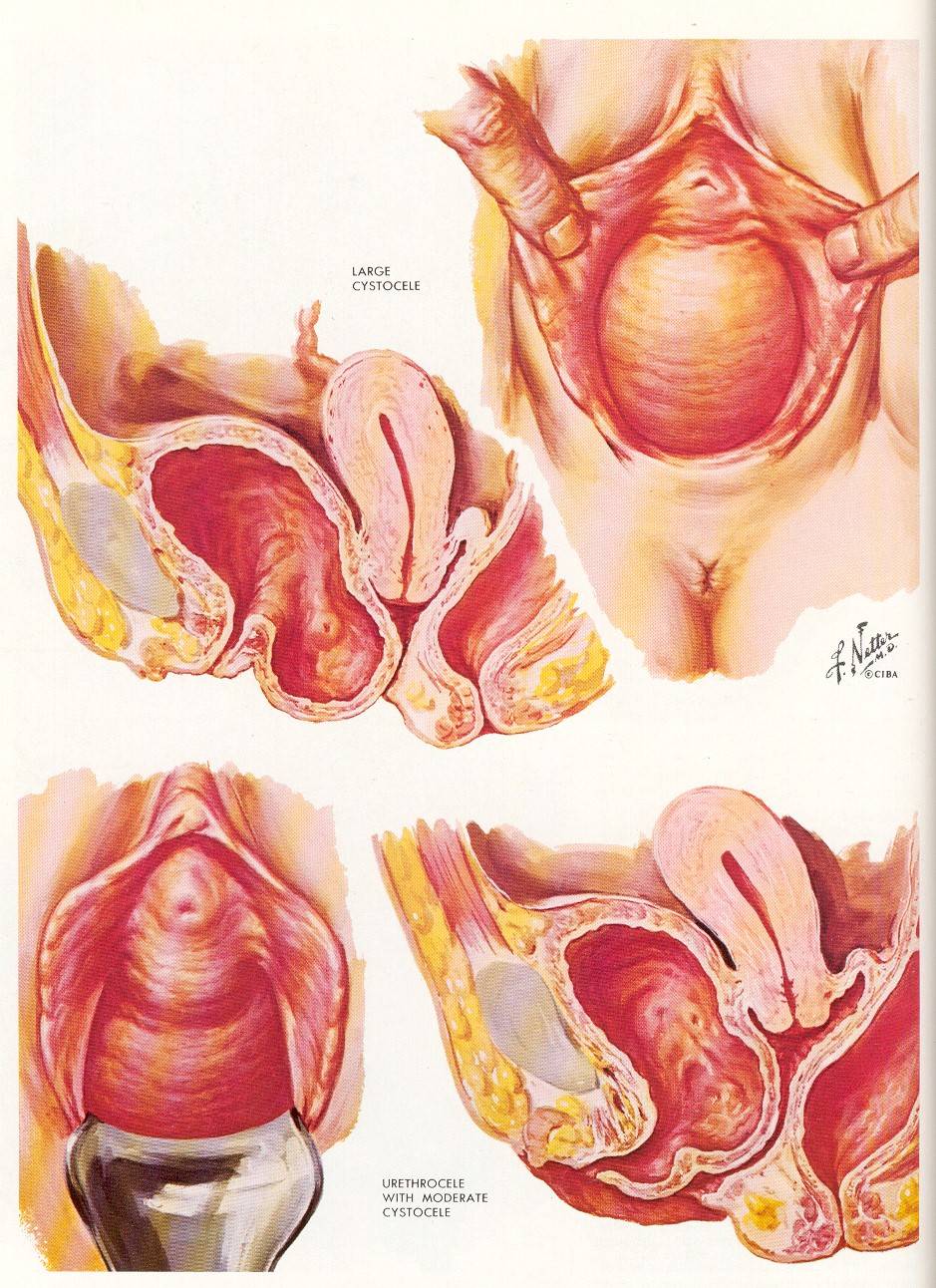
Complications can sometimes result, including ulceration of exposed tissue and prolapse of other pelvic organs such as the bladder or the rectum.
Among women aged 55 years and above, it is one of the most common reasons for undergoing a hysterectomy.
Here are some key points about uterine prolapse. More detail is in the main article.
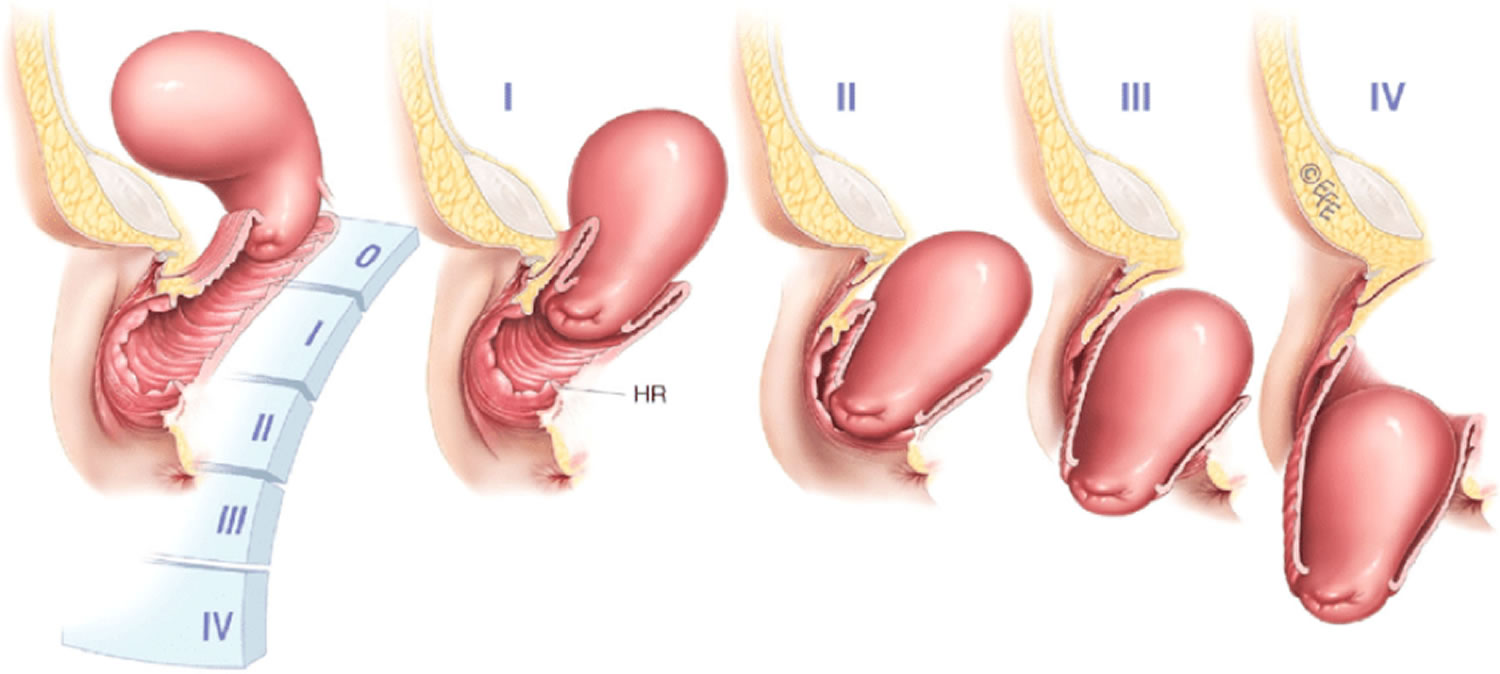
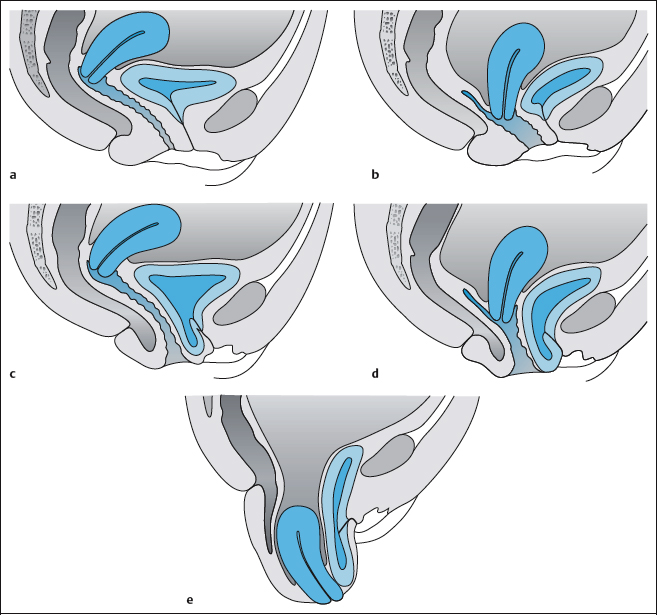
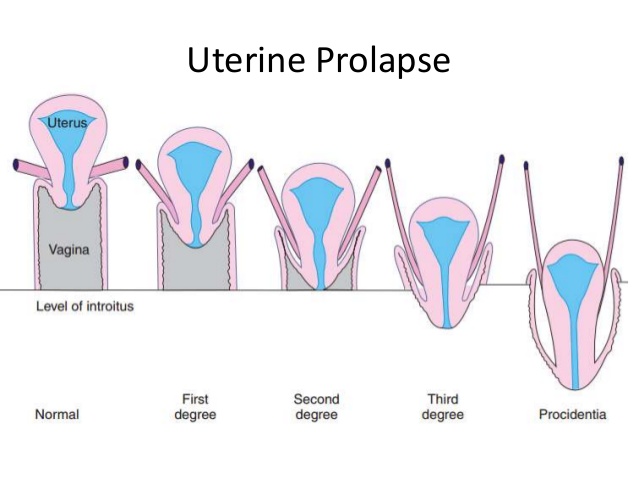
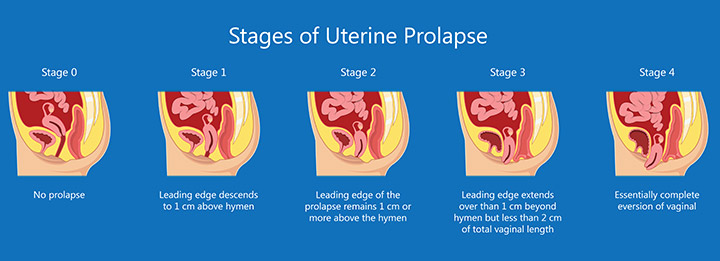
Uterine prolapse can be categorized as incomplete or complete:
The condition is graded by its severity, determined by how far the uterus has descended:
More severe cases may need surgery, but in the early stages, exercises may help.
Symptoms vary depending on how severe the prolapse is.
In mild cases, there may be no symptoms. Symptoms that appear only sometimes often become worse toward the end of the day.
Pelvic floor muscles can become weak for a number of reasons:
A health care provider will ask about symptoms and perform a physical examination. While examining the pelvis, the provider will evaluate for organ placement and vaginal tone.
An ultrasound or MRI may help assess the severity of the prolapse.
Treatment depends on the stage and severity of the prolapse.
Some strategies can reduce the risk of uterine prolapse developing and stop it from worsening.
If the prolapse shows signs of worsening, other types of treatment may be necessary.
Prolapse up to the third degree may spontaneously resolve. More severe cases may require medical treatment.
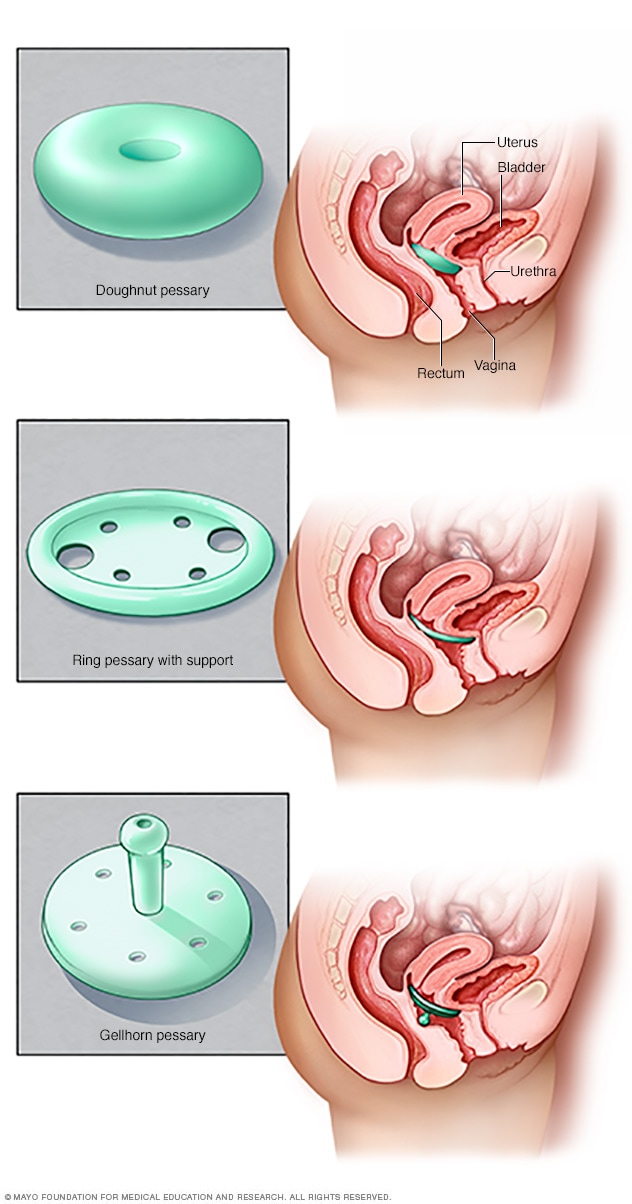
Vaginal pessary : This is a vaginal device that supports the uterus and keeps it in position. It is important to follow the instructions on care, removal, and insertion of the pessary. In cases of severe prolapse, a pessary can cause irritation, ulceration, and sexual problems. Discuss with your provider if this treatment is right for you.
Surgery : Surgical repair of a prolapsed uterus can be performed through the vagina or abdomen. It involves skin grafting, or using donor tissue or other material to provide uterine suspension. A hysterectomy may be recommended.
If future pregnancies are intended, surgery may not be recommended, due to the risks of undoing the effects of surgical repair.
Mild uterine prolapse can be treated with Kegel exercises, weight management and avoidance of heavy lifting.
How to do a proper Kegel is vital to the success of the treatment. These exercises can be done anywhere and at any time and can help strengthen the muscles of the pelvic floor.
Your health care provider or physical therapist can instruct you on how to perform a proper Kegel while in the office, at which time proper technique can be evaluated.
Sometimes, a technique called biofeedback may be applied. During biofeedback treatments, a device will monitor proper muscle contraction, the strength of the pelvic floor and timing of Kegels. This reinforces proper technique of the exercises.
The ultimate goal is to hold the contraction for 10 seconds each time the exercise is performed.
Speak with your health care provider if you have any questions or for the evaluation and treatment of symptoms of uterine prolapse. They can make recommendations on a treatment choice that is best for you.
Uterine prolapse - Symptoms and causes - Mayo Clinic
Prolapsed uterus : Stages, symptoms, and home remedies
Uterine Prolapse : Causes, Symptoms, Diagnosis & Treatment
Uterine Prolapse : Stages, Causes, Symptoms, Treatment, and Surgery
Prolapsed Uterus - Causes, Signs, Symptoms, Treatment and Exercises
Call for Additional Assistance
800.223.2273
Uterine prolapse is a common condition that can happen as a woman ages. Over time, and with multiple vaginal deliveries during childbirth, the muscles and ligaments around your uterus can weaken. When this support structure starts to fail, your uterus can sag out of position. This is called a uterine prolapse.
Appointments & Access
Contact Us
Share
The American College of Obstetricians and Gynecologists. Pelvic Support Problems . Accessed 12/30/2019.
Merck Manual Professional Version. Uterine and Apical Prolapse . Accessed 12/30/2019.
Doshani A, Teo R, Mayne C, Tincello D. Uterine prolapse . BMJ. Oct 2007; 335(7624): 819-823. Accessed 12/30/2019.
US Department of Health and Human Services, Office on Women’s Health. Pelvic Organ Prolpase . Accessed 12/30/2019.
National Health Service. Pelvic Organ Prolapse . Accessed 12/30/2019.
Get useful, helpful and relevant health + wellness information
Cleveland Clinic’s Ob/Gyn & Women’s Health Institute is committed to providing world-class care for women of all ages. We offer women's health services, obstetrics and gynecology throughout Northeast Ohio and beyond. Whether patients are referred to us or already have a Cleveland Clinic ob/gyn, we work closely with them to offer treatment recommendations and follow-up care to help you receive the best outcome.
The Glickman Urological & Kidney Institute offers innovative treatments in urology and nephrology, including minimally invasive, scarless options for urologic procedures and medical management of kidney disease.
Appointments & Access
Contact Us
Actions
Appointments & Access Pay Your Bill Financial Assistance Accepted Insurance Make a Donation Refer a Patient Phone Directory Events Calendar
Blog, News & Mobile Apps
Consult QD Health Essentials Newsroom Mobile Apps
9500 Euclid Avenue, Cleveland, Ohio 44195 | 800.223.2273 | © 2021 Cleveland Clinic. All Rights Reserved.
A uterine prolapse is a condition where the internal supports of the uterus become weak over time. The uterus is one of the organs that makes up part of your reproductive system. Also called the womb, the uterus is located in your pelvis and is roughly shaped like a pear. During pregnancy, the uterus holds the developing baby. It actually stretches through the pregnancy to fit the baby and then shrinks back down in size after delivery.
Prolapses can vary depending on how weak the supports of the uterus have gotten. In an incomplete prolapse, the uterus may have slipped enough to be partway in the vagina (birth canal). This creates a lump or bulge. In a more severe case, the uterus can slip far enough that it is felt outside of the vagina. This is called a complete prolapse.
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services.
Policy
Uterine prolapse is most likely to happen in women who:
Menopause occurs when your ovaries stop producing the hormones that regulate your monthly menstrual cycle (period). When you haven’t had a period for 12 straight months, you are considered menopausal. One of the hormones that stops during menopause is estrogen. This particular hormone helps keep your pelvic muscles strong. Without it, you are at a higher risk of developing a prolapse.
Uterine prolapse is a fairly common condition. Your risk of developing the condition increases with age. You are also at a higher risk of uterine prolapses if you have had multiple vaginal deliveries during childbirth throughout your life.
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services.
Policy
Your uterus is held in place within the pelvis by a group of muscles and ligaments. You may hear this called the pelvic floor muscles. When these structures weaken, they become unable to hold the uterus in position, and it begins to sag. Several factors can contribute to the weakening of the pelvic muscles, including:
If you have a mild case of uterine prolapse, you may not have any obvious symptoms. However, as the uterus slips further out of position, it can place pressure on other pelvic organs—such as the bladder or bowel—and cause symptoms like:
Symptoms can get worse when you stand or walk for long periods of time. In these positions, gravity places extra pressure on the pelvic muscles.
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services.
Policy
The healthcare provider will perform a pelvic examination to determine if the uterus has lowered from its normal position. During a pelvic exam, the healthcare provider inserts a speculum (an instrument that lets the provider see inside the vagina) and examines the vagina and uterus. Your provider will feel for any bulges caused by the uterus dropping down into the vaginal canal.
There are surgical and non-surgical options for treating uterine prolapse. Your healthcare provider will pick your treatment path based on the severity of your prolapse, your general health, age and whether or not you want children in the future. Treatment is generally effective for most women. Treatment options can include:
If you don’t treat a uterine prolapse, it can impact other organs in the pelvic area of your body. A prolapsed uterus can interfere with your bowel and bladder. It can also negatively impact your sex life, causing you pain.
You may not be able to prevent all cases of uterine prolapse, but there are ways to cut back on your risk of developing a prolapse. A few lifestyle tips that can reduce your risk of prolapse include:
There are several tips for lifting heavy objects that can help you avoid injury. These techniques for lifting include:
Most of the time, treatment for a uterine prolapse is effective. However, sometimes a prolapse can come back. This is more common if you have a very severe prolapse, are obese or a younger woman (under age 60).
In most cases, the outlook for uterine prolapse is very good. There are typically very positive results from treatment for the condition and lifestyle changes (maintaining a good weight and exercising) can help prevent a prolapse from happening again. Talk to your healthcare provider about any concerns you may have about prolapses. Your provider can help you develop a treatment plan and build good lifestyle habits to prevent any future prolapses.
Last reviewed by a Cleveland Clinic medical professional on 12/30/2019.
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services.
Policy
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services.
Policy
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services.
Policy
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services.
Policy
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services.
Policy