Uterine Prolapse
⚡ ALL INFORMATION CLICK HERE 👈🏻👈🏻👈🏻
Uterine Prolapse
Medically reviewed by Holly Ernst, PA-C — Written by Jaime Herndon, MS, MPH, MFA — Updated on September 17, 2018
Medically reviewed by Holly Ernst, PA-C — Written by Jaime Herndon, MS, MPH, MFA — Updated on September 17, 2018
Medically reviewed by Graham Rogers, M.D.
Medically reviewed by William Morrison, M.D.
Medically reviewed by Beth Holloway, RN, MEd
© 2005-2021 Healthline Media a Red Ventures Company. All rights reserved. Our website services, content, and products are for informational purposes only. Healthline Media does not provide medical advice, diagnosis, or treatment. See additional information .
© 2005-2021 Healthline Media a Red Ventures Company. All rights reserved. Our website services, content, and products are for informational purposes only. Healthline Media does not provide medical advice, diagnosis, or treatment. See additional information .
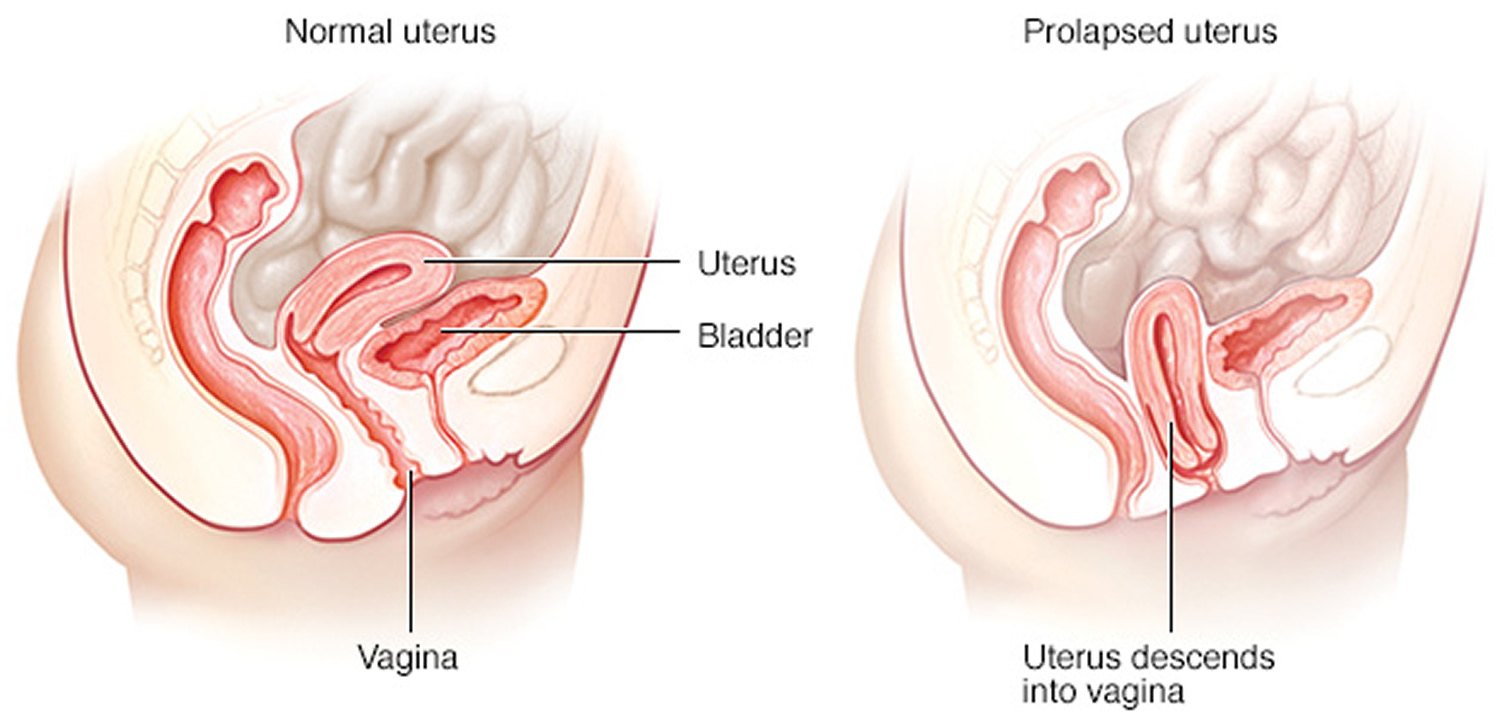
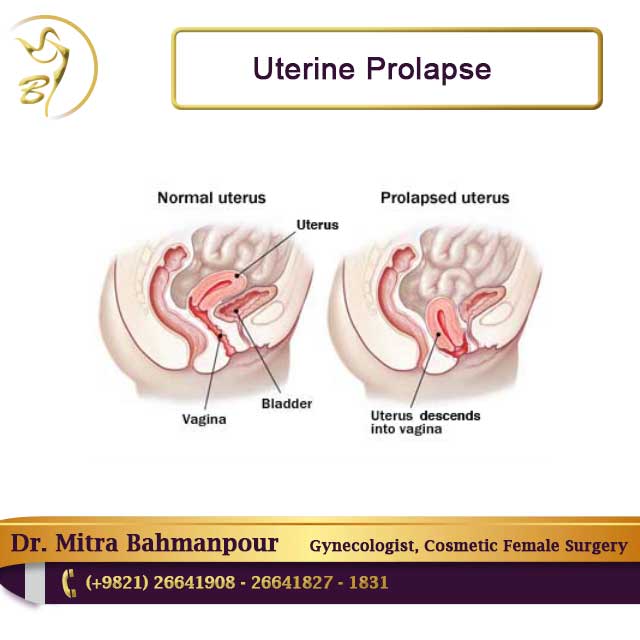
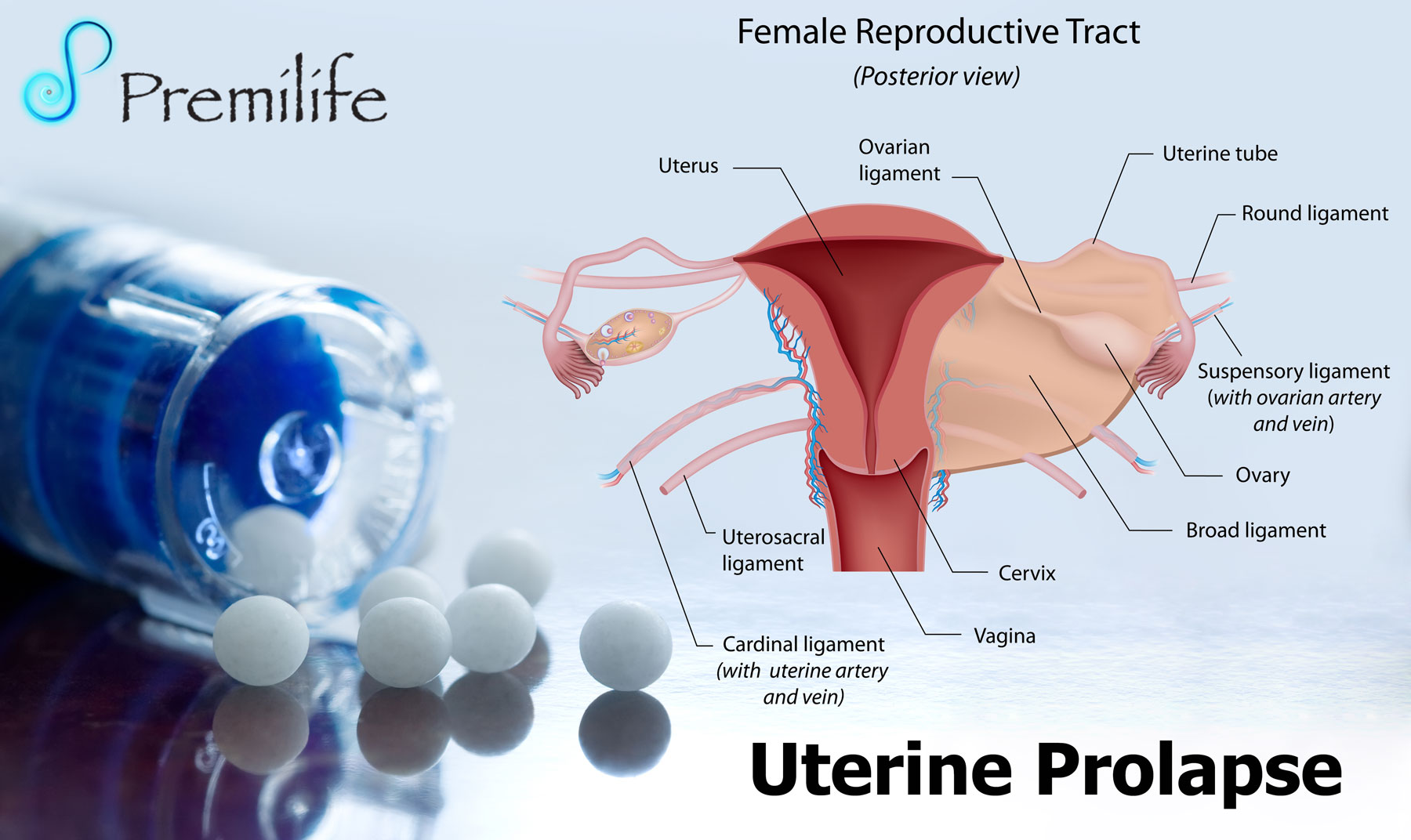
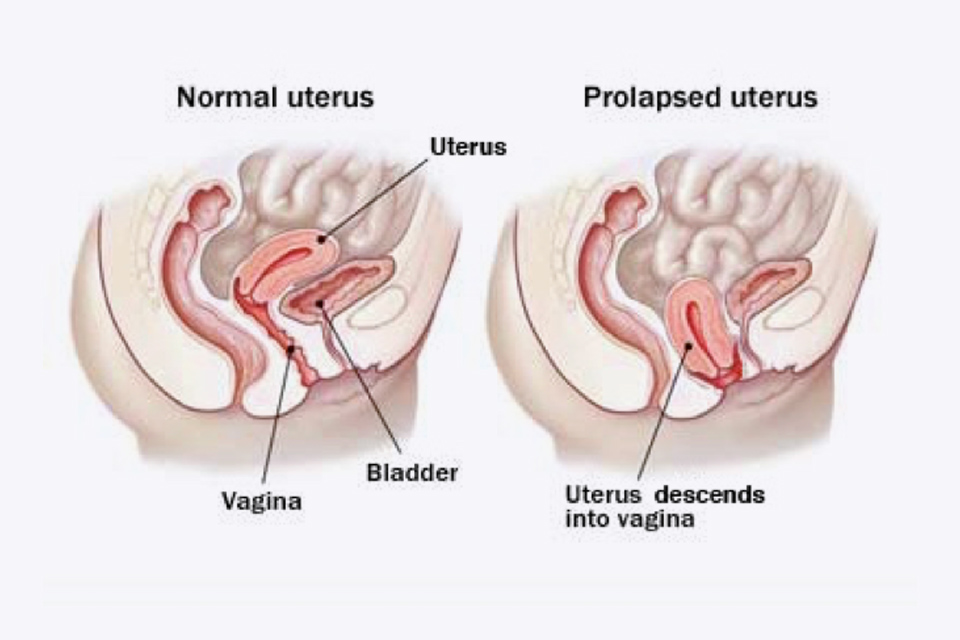
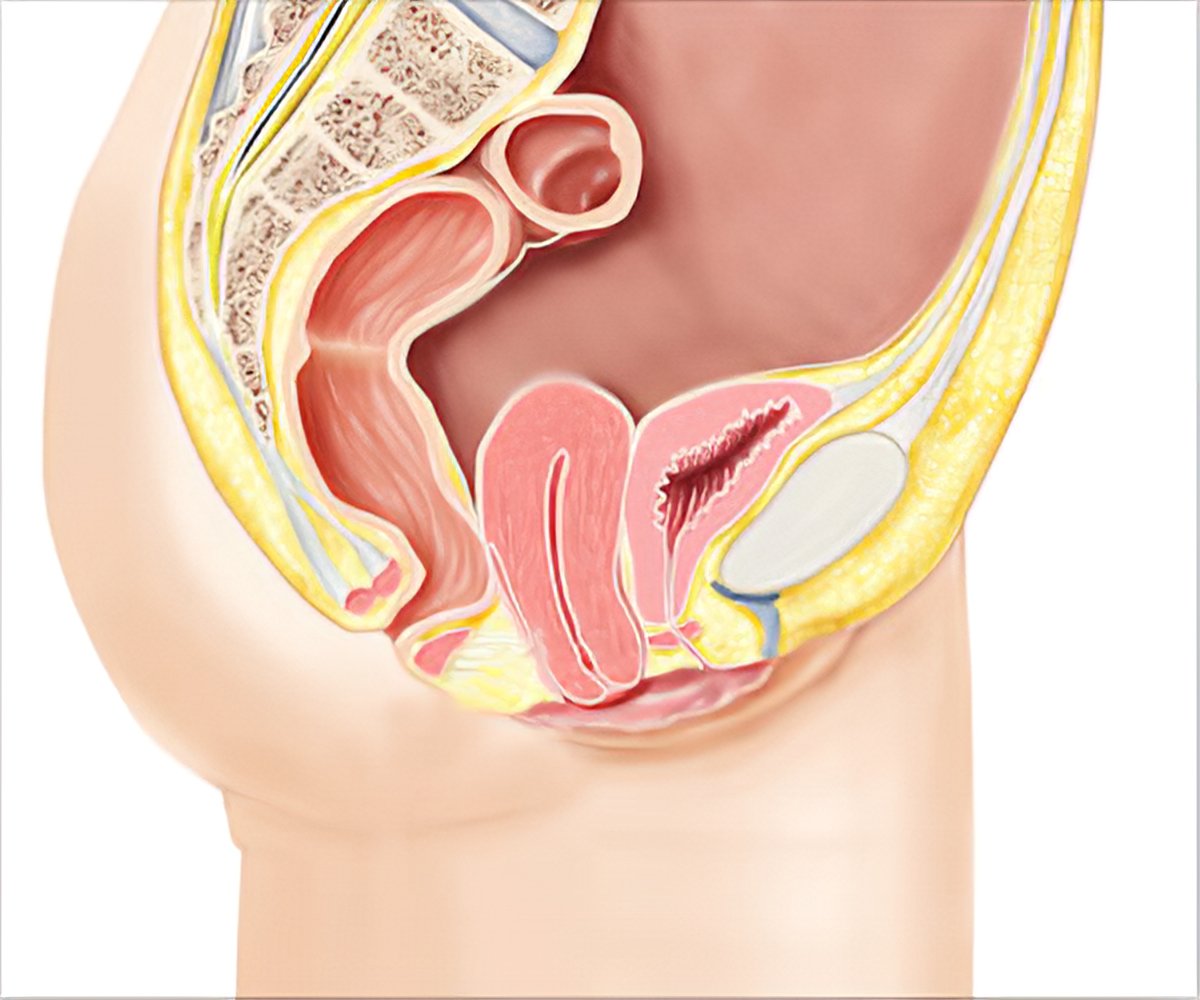
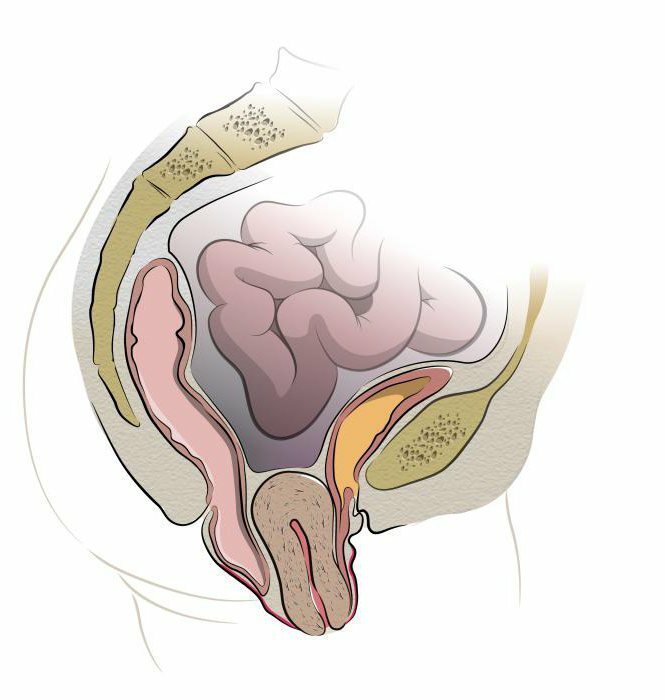
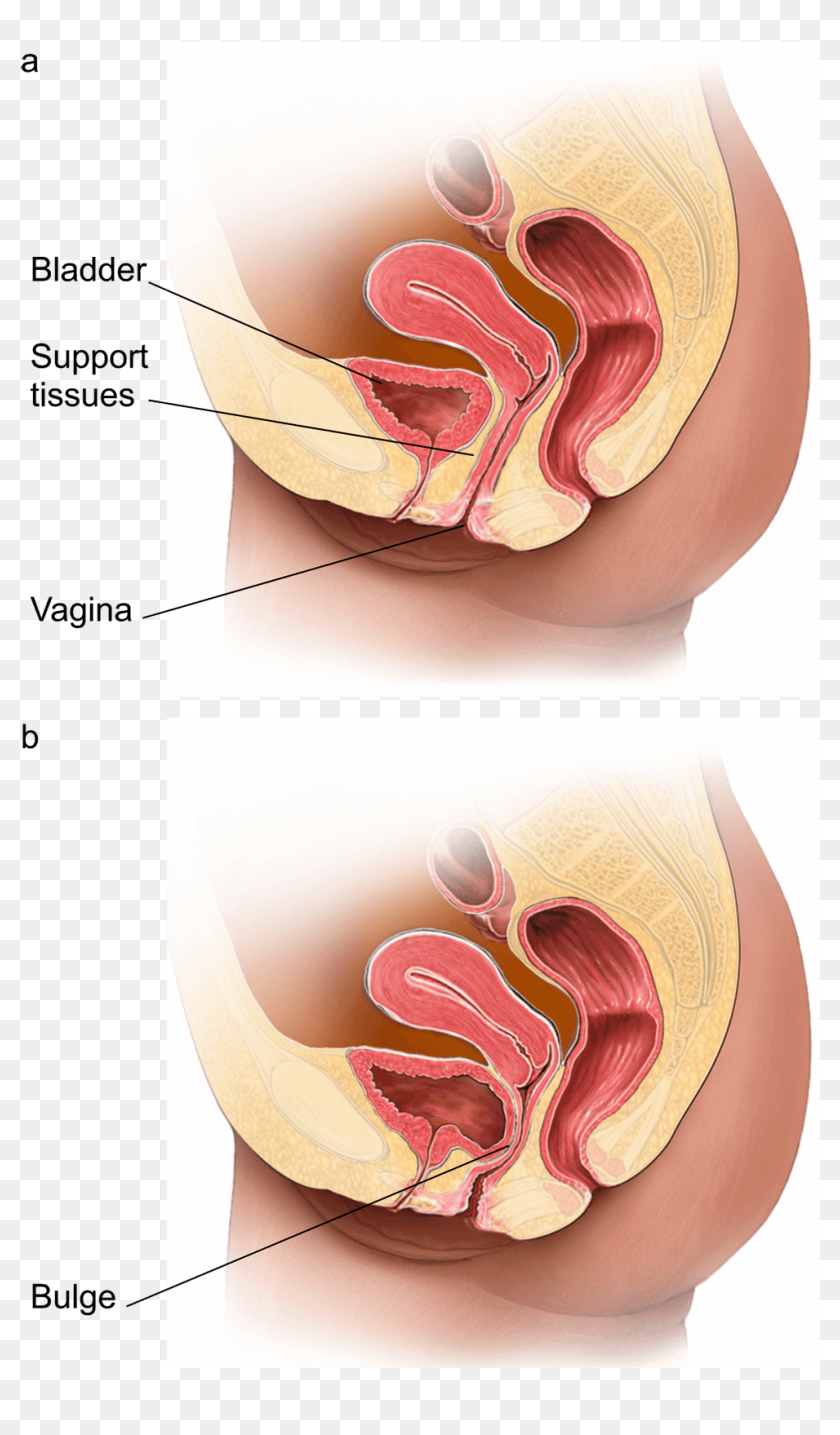
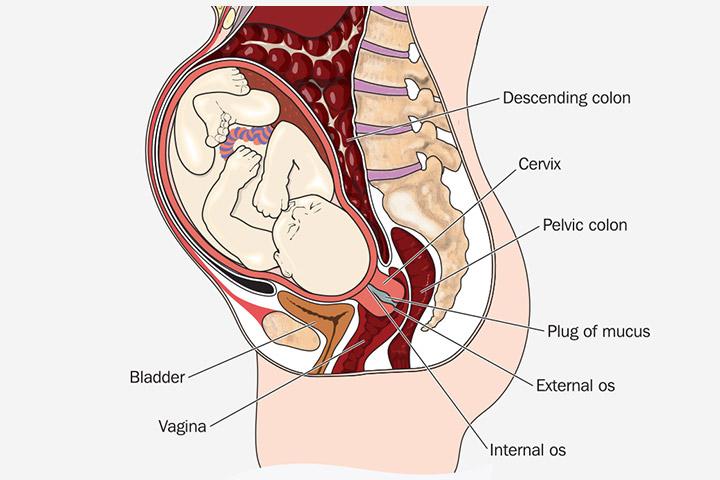
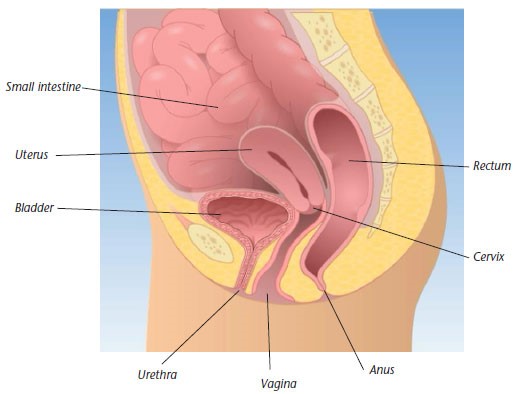
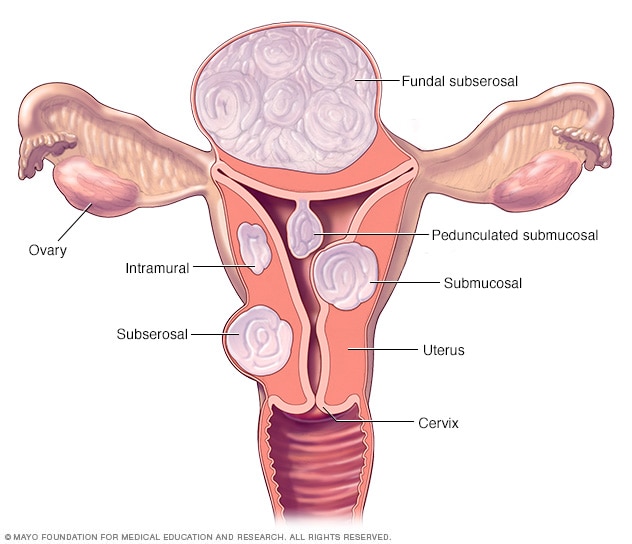
The uterus (womb) is a muscular structure that’s held in place by pelvic muscles and ligaments. If these muscles or ligaments stretch or become weak, they’re no longer able to support the uterus, causing prolapse.
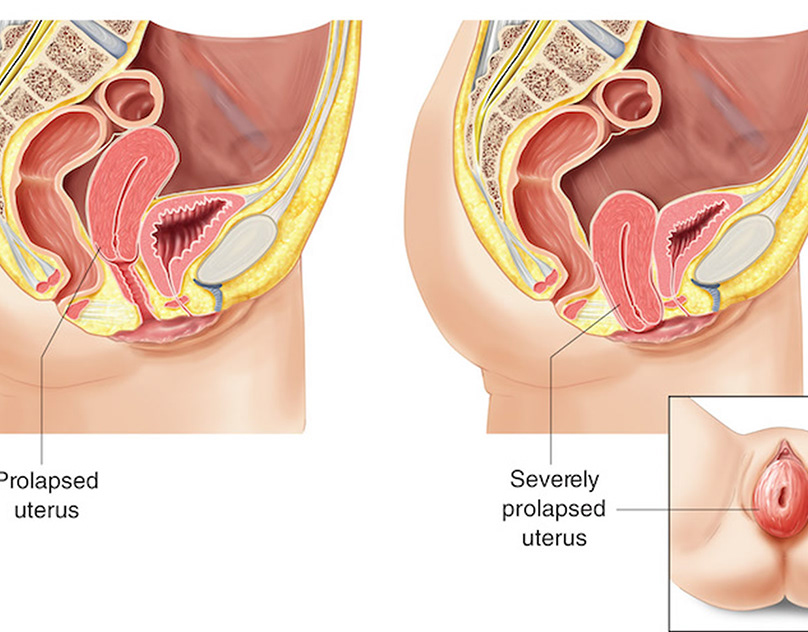
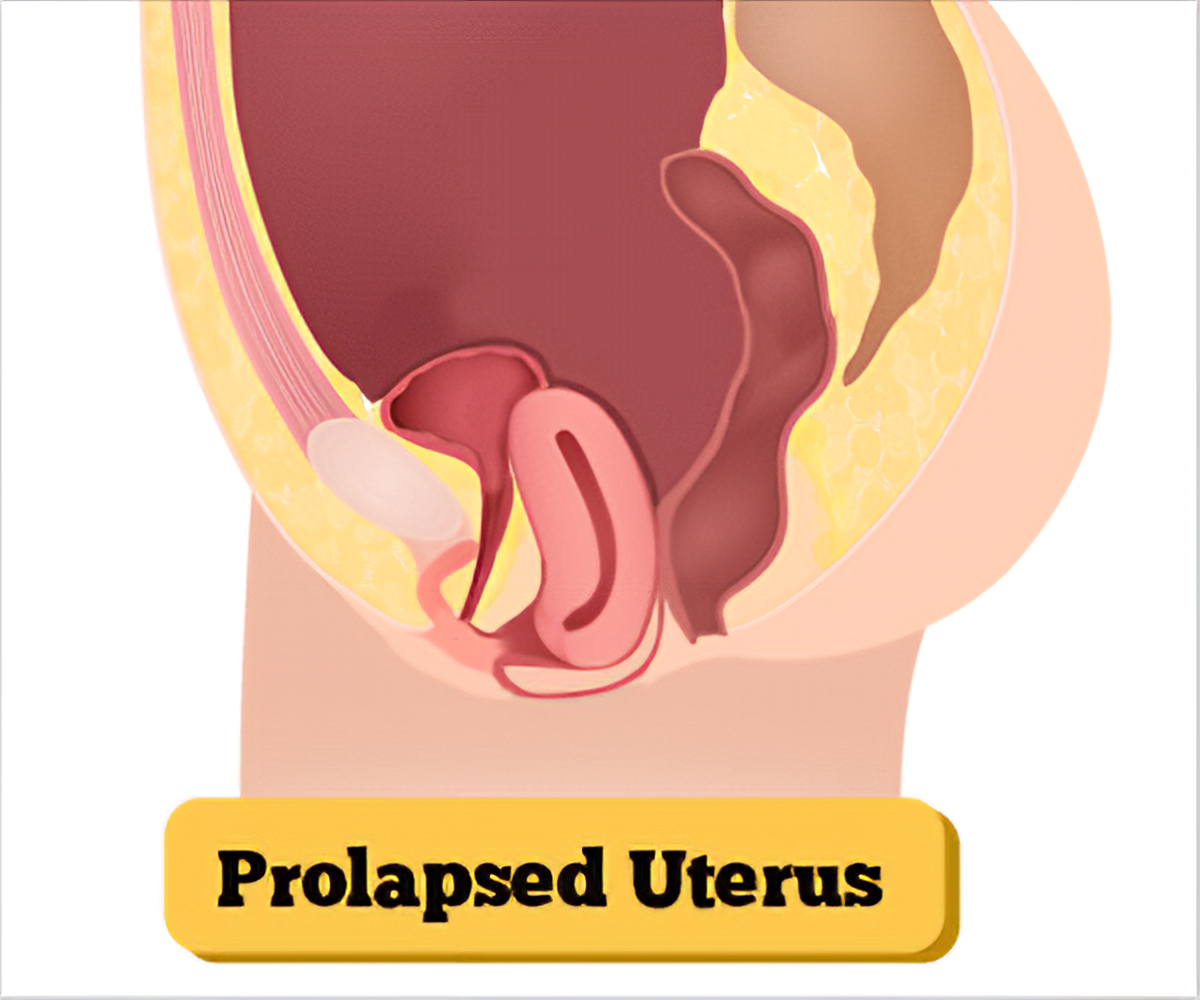
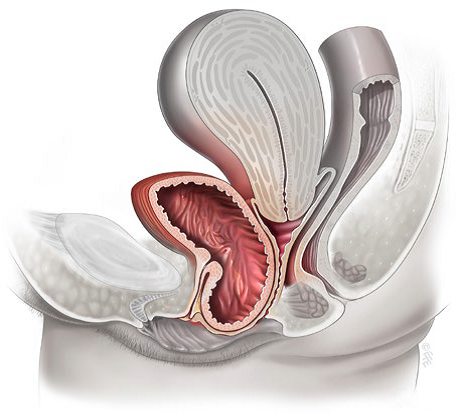
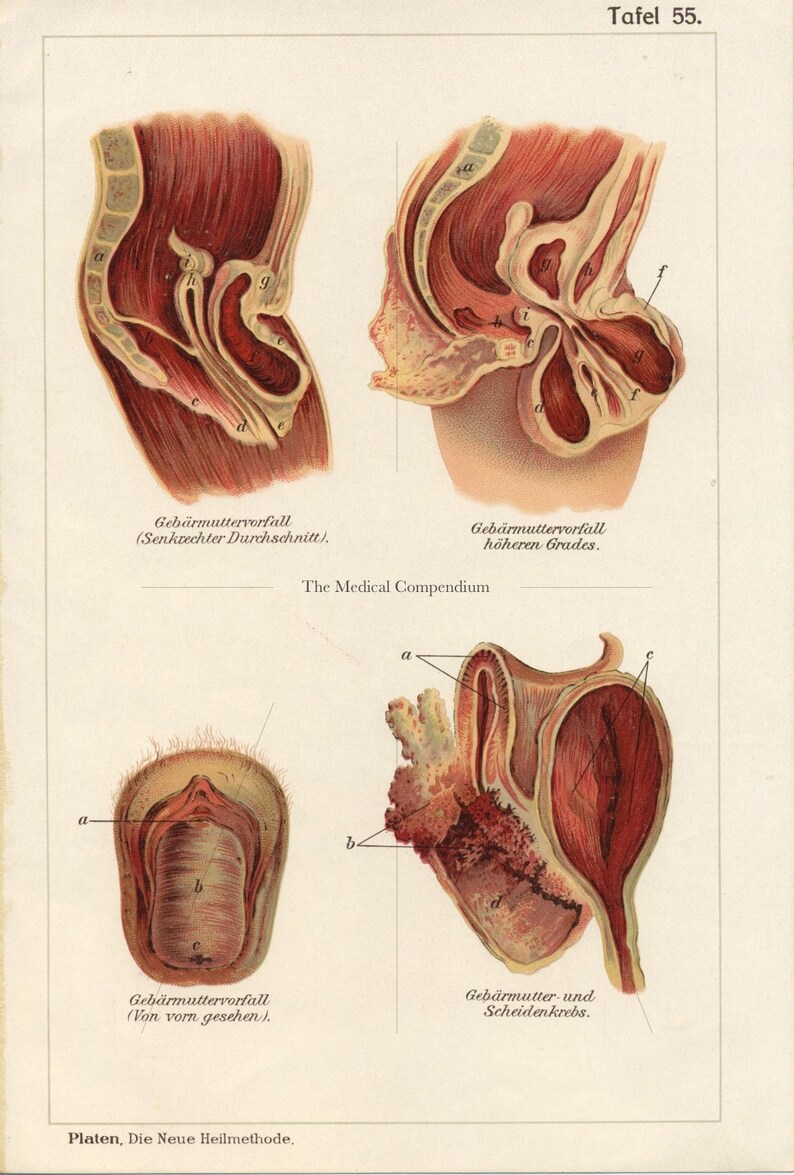
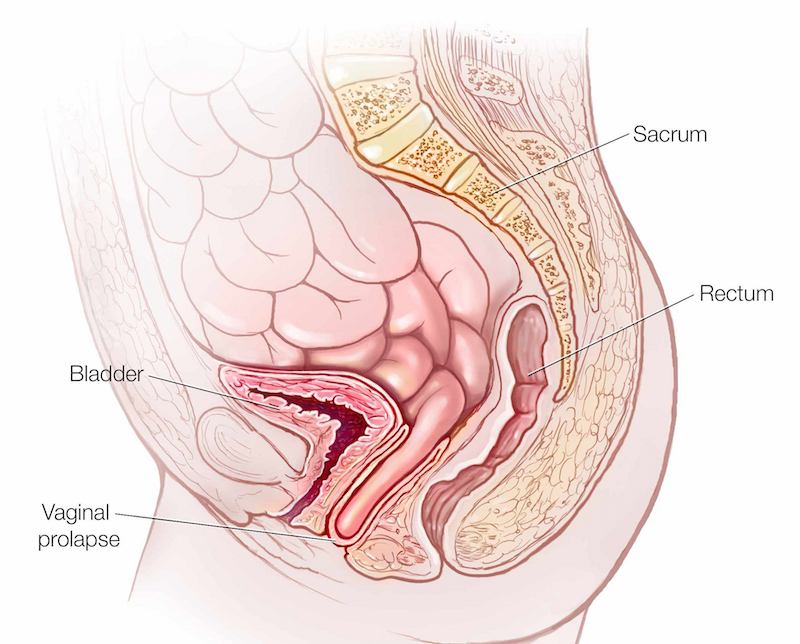
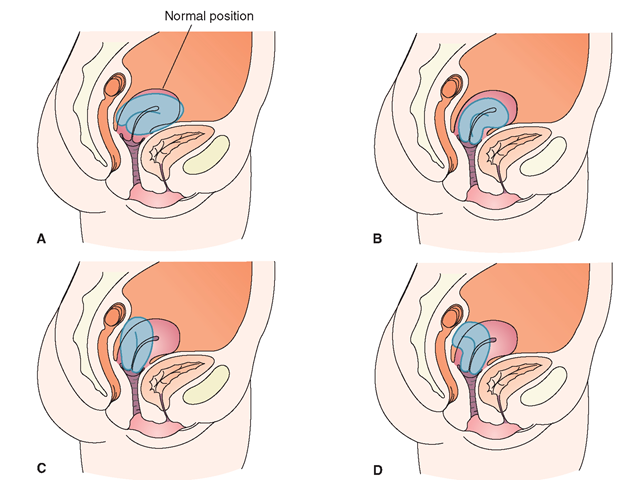
Uterine prolapse occurs when the uterus sags or slips from its normal position and into the vagina (birth canal).
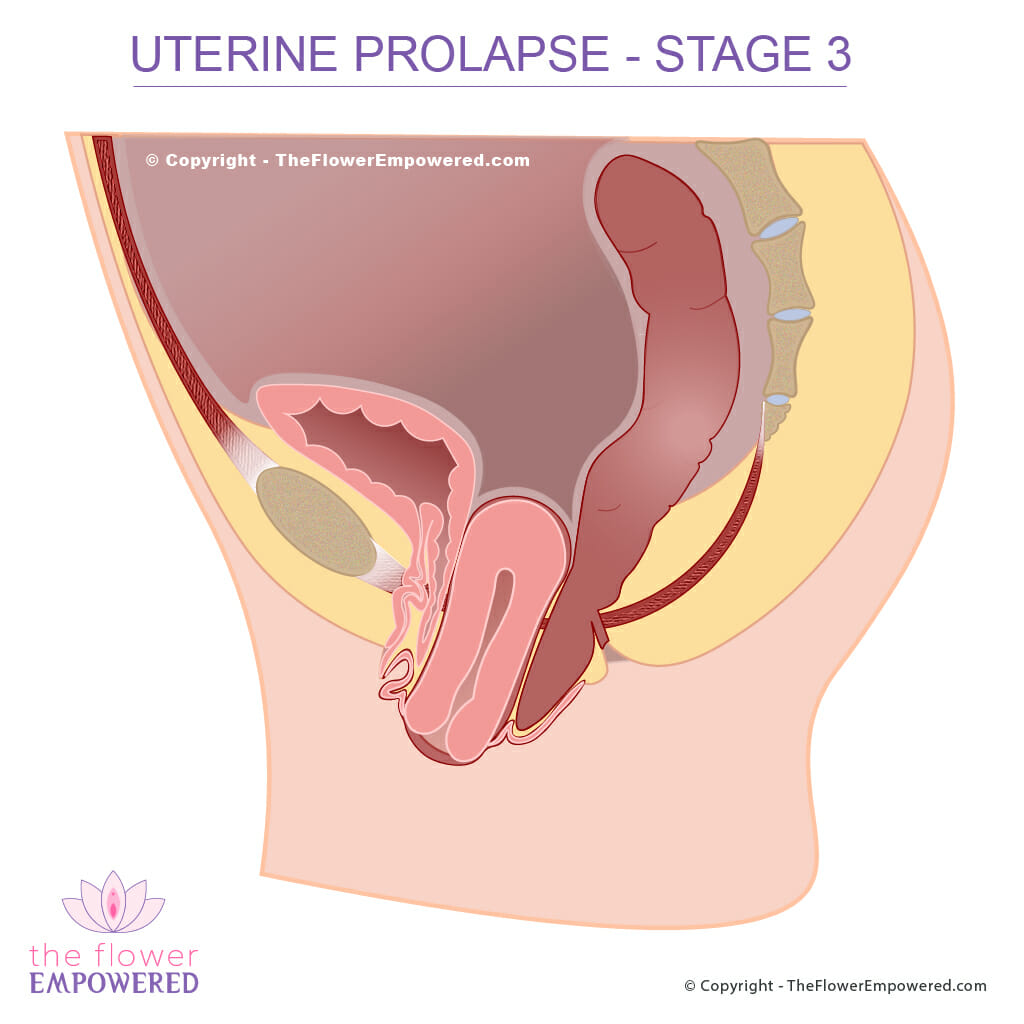
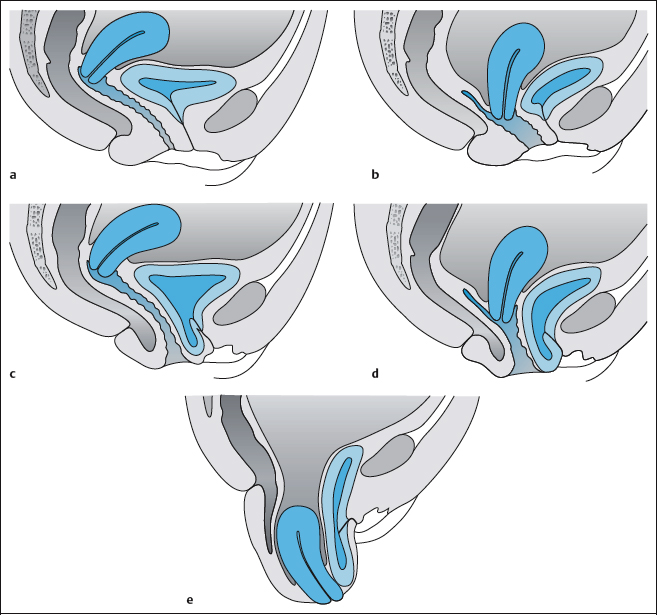
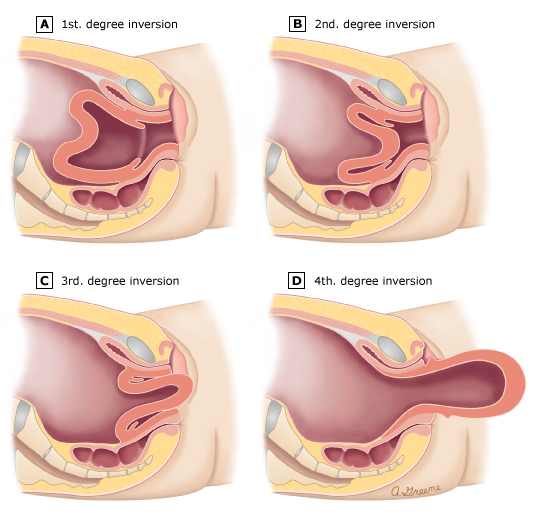
Uterine prolapse may be incomplete or complete. An incomplete prolapse occurs when the uterus is only partly sagging into the vagina. A complete prolapse occurs when the uterus falls so far down that some tissue protrudes outside of the vagina.
Women who have a minor uterine prolapse may not have any symptoms. Moderate to severe prolapse may cause symptoms, such as:
If you develop these symptoms, you should see your doctor and get treatment right away. Without proper attention, the condition can impair your bowel, bladder, and sexual function.
The risk of having a prolapsed uterus increases as a woman ages and her estrogen levels decrease. Estrogen is the hormone that helps keep the pelvic muscles strong. Damage to pelvic muscles and tissues during pregnancy and childbirth may also lead to prolapse. Women who’ve had more than one vaginal birth or are postmenopausal are at the highest risk.
Any activity that puts pressure on the pelvic muscles can increase your risk of a uterine prolapse. Other factors that can increase your risk for the condition include:
Your doctor can diagnose uterine prolapse by evaluating your symptoms and performing a pelvic exam . During this exam, your doctor will insert a device called a speculum that allows them to see inside of the vagina and examine the vaginal canal and uterus. You may be lying down, or your doctor may ask you to stand during this exam.
Your doctor may ask you to bear down as if you’re having a bowel movement to determine the degree of prolapse.
Treatment isn’t always necessary for this condition. If the prolapse is severe, talk with your doctor about which treatment option is appropriate for you.
The use of vaginal estrogen has been well-studied and shows improvement in vaginal tissue regeneration and strength. While using vaginal estrogen to help augment other treatment options may be helpful, on its own it doesn’t reverse the presence of a prolapse.
Surgical treatments include uterine suspension or hysterectomy . During uterine suspension, your surgeon places the uterus back into its original position by reattaching pelvic ligaments or using surgical materials. During a hysterectomy, your surgeon removes the uterus from the body through the abdomen or the vagina.
Surgery is often effective, but it’s not recommended for women who plan on having children. Pregnancy and childbirth can put an immense strain on pelvic muscles, which can undo surgical repairs of the uterus.
Uterine prolapse may not be preventable in every situation. However, you can do several things to reduce your risk, including:
Last medically reviewed on September 17, 2018
Uterine Prolapse : Stages, Causes, Symptoms, Treatment, and Surgery
Uterine Prolapse : Risk Factors, Symptoms, and Diagnosis
Uterine prolapse : MedlinePlus Medical Encyclopedia
Uterine Prolapse - an overview | ScienceDirect Topics
Uterine and Apical Prolapse - Gynecology and Obstetrics - MSD Manual...
The navigation menu has been collapsed.
About MedlinePlus
What's New
Site Map
Customer Support
COVID-19 is an emerging, rapidly evolving situation.
Get the latest public health information from CDC: https://www.coronavirus.gov Get the latest research information from NIH: https://covid19.nih.gov Learn more about COVID-19 and you from HHS: https://combatcovid.hhs.gov
When to Contact a Medical Professional
About MedlinePlus
What's New
Site Map
Customer Support
Get updates
Subscribe to RSS
Follow us
Social Media Toolkit
Page last updated: 26 February 2021
Uterine prolapse occurs when the womb (uterus) drops down and presses into the vaginal area.
Muscles, ligaments, and other structures hold the uterus in the pelvis. If these tissues are weak or stretched, the uterus drops into the vaginal canal. This is called prolapse.
This condition is more common in women who have had 1 or more vaginal births.
Other things that can cause or lead to uterine prolapse include:
Repeated straining to have a bowel movement due to long-term constipation can make the problem worse.
Symptoms may be worse when you stand or sit for a long time. Exercise or lifting may also make symptoms worse.
Your health care provider will do a pelvic exam. You will be asked to bear down as if you are trying to push out a baby. This shows how far your uterus has dropped.
Other things the pelvic exam may show are:
You do not need treatment unless you are bothered by the symptoms.
Many women will get treatment by the time the uterus drops to the opening of the vagina.
The following can help you control your symptoms:
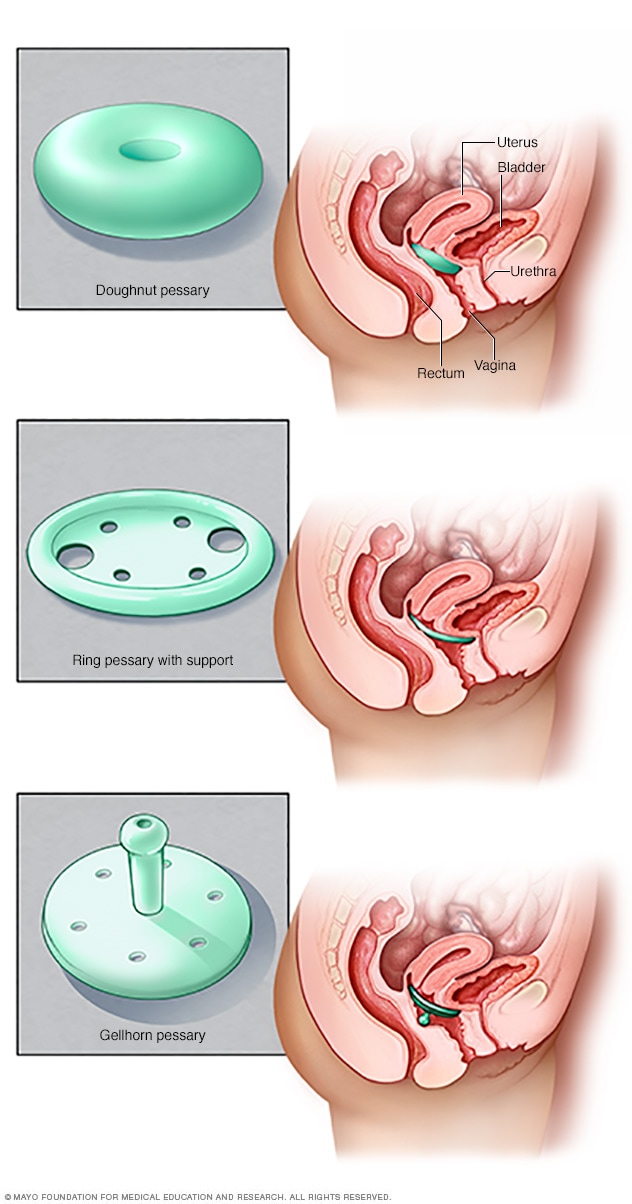
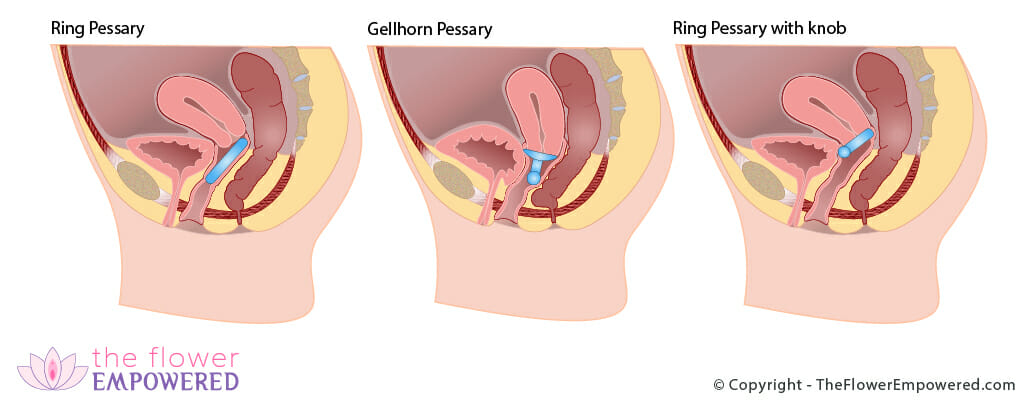
Your provider may recommend placing a rubber or plastic donut-shaped device, into the vagina. This is called a pessary. This device holds the uterus in place.
The pessary may be used for short-term or long-term. The device is fitted for your vagina. Some pessaries are similar to a diaphragm used for birth control.
Pessaries must be cleaned regularly. Sometimes they need to be cleaned by the provider. Many women can be taught how to insert, clean, and remove a pessary.
Surgery should not be done until the prolapse symptoms are worse than the risks of having surgery. The type of surgery will depend on:
There are some surgical procedures that can be done without removing the uterus, such as a sacrospinous fixation. This procedure involves using nearby ligaments to support the uterus. Other procedures are also available.
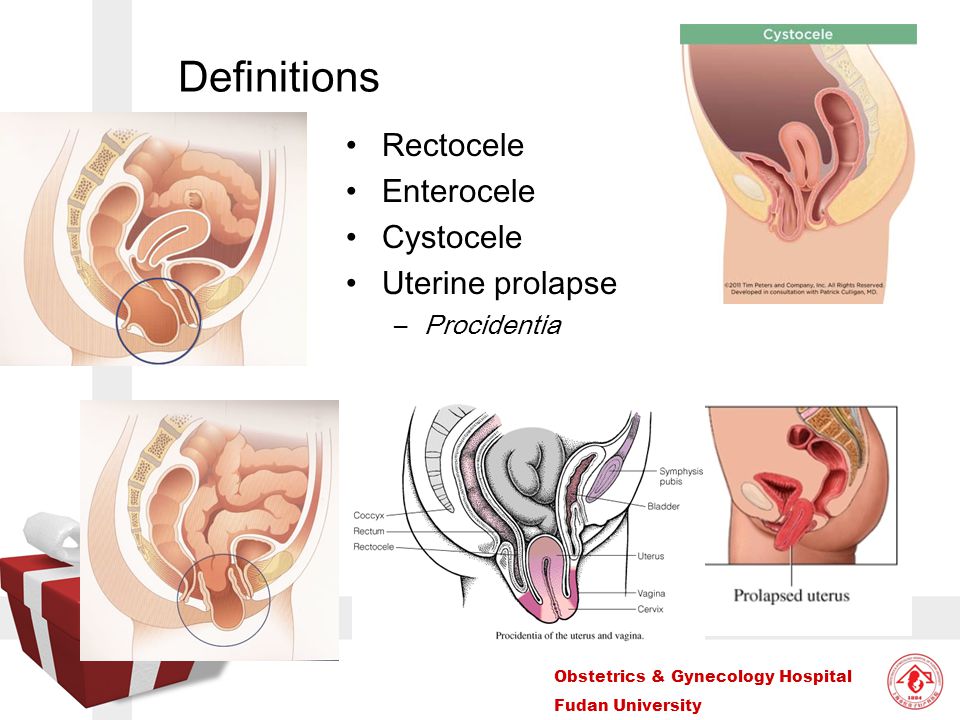
Often, a vaginal hysterectomy can be done at the same time as the procedure to correct uterine prolapse. Any sagging of the vaginal walls, urethra, bladder, or rectum can be surgically corrected at the same time.
Most women with mild uterine prolapse do not have symptoms that require treatment.
Vaginal pessaries can be effective for many women with uterine prolapse.
Surgery often provides very good results. However, some women may need to have the treatment again in the future.
Ulceration and infection of the cervix and vaginal walls may occur in severe cases of uterine prolapse.
Urinary tract infections and other urinary symptoms may occur because of a cystocele. Constipation and hemorrhoids may occur because of a rectocele.
Call your provider if you have symptoms of uterine prolapse.
Tightening the pelvic floor muscles using Kegel exercises helps to strengthen the muscles and reduces the risk of developing uterine prolapse.
Estrogen therapy after menopause may help with vaginal muscle tone.
Pelvic relaxation - uterine prolapse; Pelvic floor hernia; Prolapsed uterus; Incontinence - prolapse
Kirby AC, Lentz GM. Anatomic defects of the abdominal wall and pelvic floor: abdominal hernias, inguinal hernias, and pelvic organ prolapse: diagnosis and management. In: Lobo RA, Gershenson DM, Lentz GM, Valea FA, eds. Comprehensive Gynecology . 7th ed. Philadelphia, PA: Elsevier; 2017:chap 20.
Magowan BA, Owen P, Thomson A. Pelvic organ prolapse. In: Magowan BA, Owen P, Thomson A, eds. Clinical Obstetrics and Gynaecology . 4th ed. Philadelphia, PA: Elsevier; 2019:chap 10.
Newman DK, Burgio KL. Conservative management of urinary incontinence: behavioral and pelvic floor therapy and urethral and pelvic devices. In: Wein AJ, Kavoussi LR, Partin AW, Peters CA, eds. Campbell-Walsh Urology . 11th ed. Philadelphia, PA: Elsevier; 2016:chap 80.
Winters JC, Smith AL, Krlin RM. Vaginal and abdominal reconstructive surgery for pelvic organ prolapse. In: Wein AJ, Kavoussi LR, Partin AW, Peters CA, eds. Campbell-Walsh Urology . 11th ed. Philadelphia, PA: Elsevier; 2016:chap 83.
Updated by: John D. Jacobson, MD, Professor of Obstetrics and Gynecology, Loma Linda University School of Medicine, Loma Linda Center for Fertility, Loma Linda, CA. Also reviewed by David Zieve, MD, MHA, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.
A.D.A.M., Inc. is accredited by URAC , for Health Content Provider (www.urac.org). URAC's accreditation program is an independent audit to verify that A.D.A.M. follows rigorous standards of quality and accountability. A.D.A.M. is among the first to achieve this important distinction for online health information and services. Learn more about A.D.A.M.'s editorial policy editorial process and privacy policy . A.D.A.M. is also a founding member of Hi-Ethics. This site complies with the HONcode standard for trustworthy health information: verify here .
The information provided herein should not be used during any medical emergency or for the diagnosis or treatment of any medical condition. A licensed physician should be consulted for diagnosis and treatment of any and all medical conditions. Call 911 for all medical emergencies. Links to other sites are provided for information only -- they do not constitute endorsements of those other sites. Copyright 1997-2021, A.D.A.M., Inc. Duplication for commercial use must be authorized in writing by ADAM Health Solutions.