Tears Anal Pain
👉🏻👉🏻👉🏻 ALL INFORMATION CLICK HERE 👈🏻👈🏻👈🏻
Now scheduling COVID-19 vaccine appointments for ages 12+
Schedule a vaccine appointment
COVID-19 vaccine FAQs
Call for Additional Assistance 800.223.2273
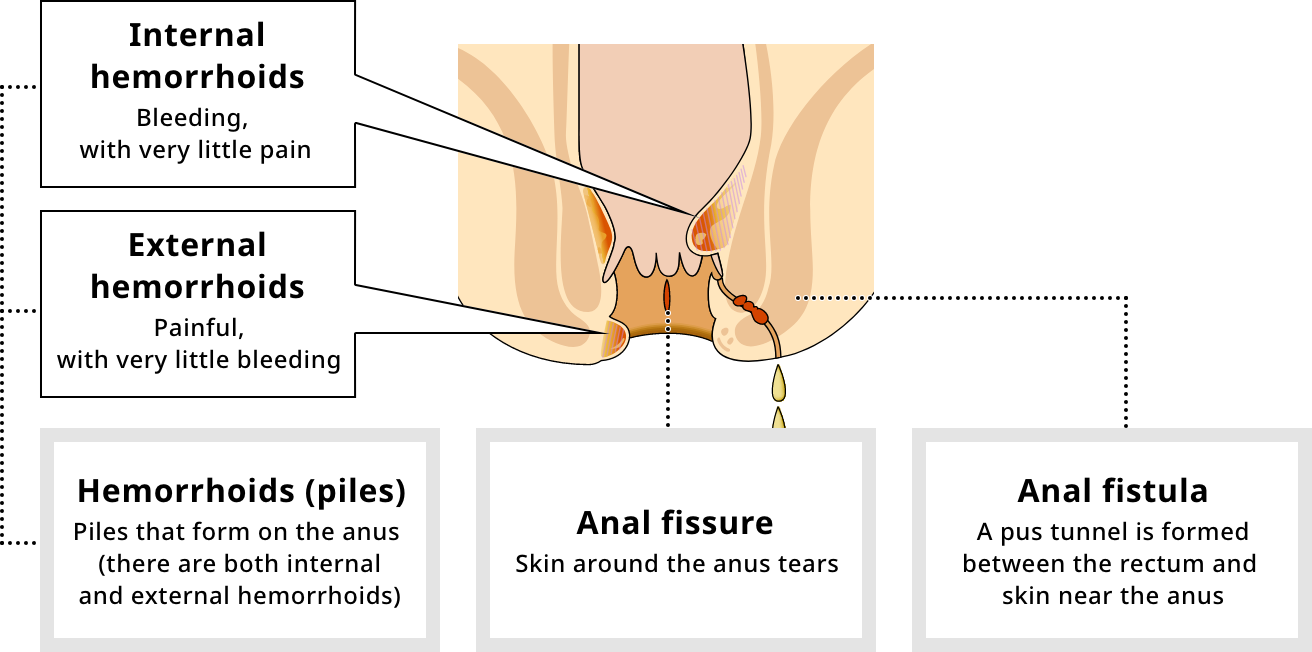
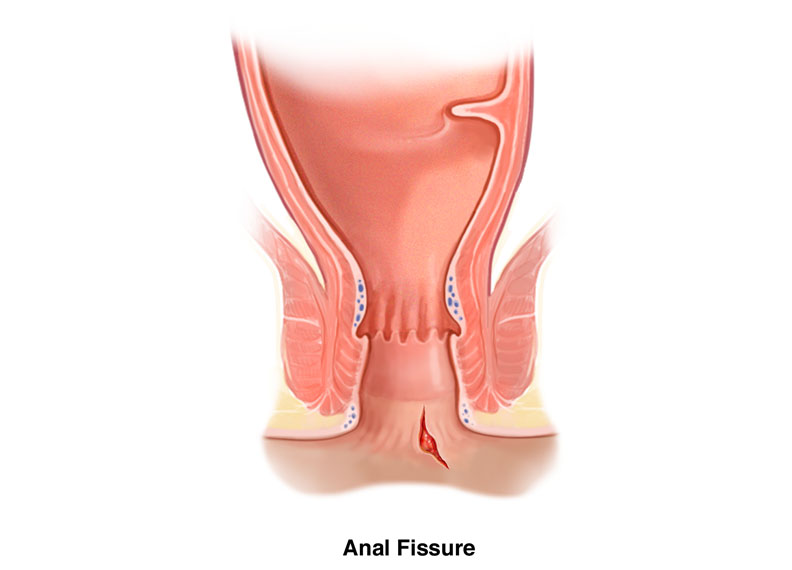
An anal fissure is a tear in the lining of the anus or anal canal. One sign of an anal fissure is pain during or after a bowel movement. Causes, diagnosis and treatment--including surgery--are discussed.
An anal fissure is a tear in the lining of the anus or anal canal (the opening through which stool passes out of the body). The fissure can be painful and may bleed.
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Anal fissures can occur in anyone at any age. The chance of having an anal fissure decreases as people get older. People who have had fissures in the past are more likely to have them in the future.
Anal fissures can be caused by trauma to the anus and anal canal. The trauma can be caused by one or more of the following:
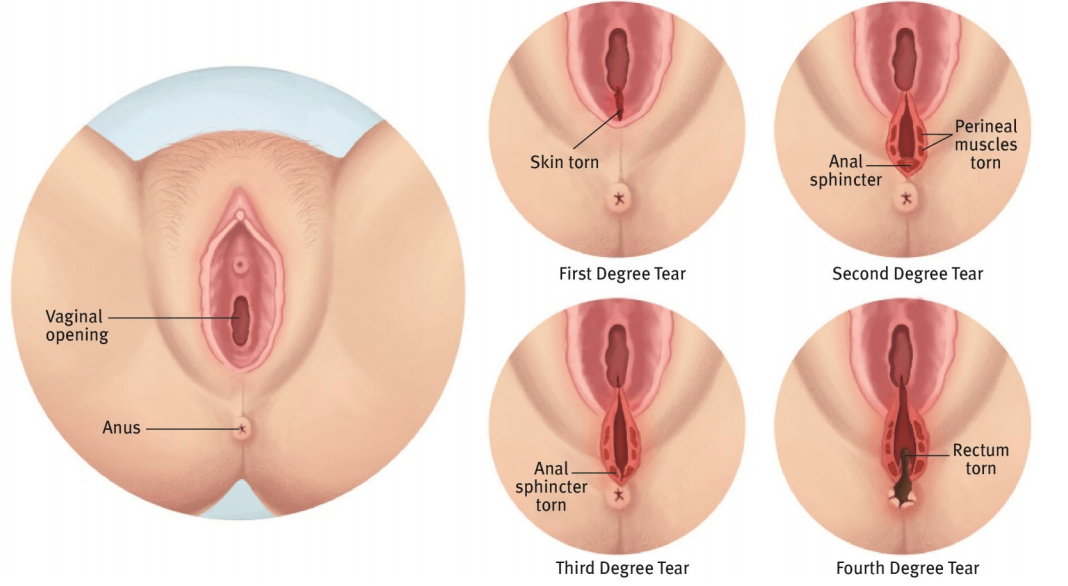
Anal fissures are also common in young infants and in women after childbirth.
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Signs and symptoms of an anal fissure include:
Usually, your doctor can diagnose an anal fissure by visual inspection of the anus or by gentle exam with the tip of the finger.
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
The goal of anal fissure treatment is to lower the pressure on the anal canal by making stools soft, and to ease discomfort and bleeding. Conservative treatments are tried first and include one or more of the following:
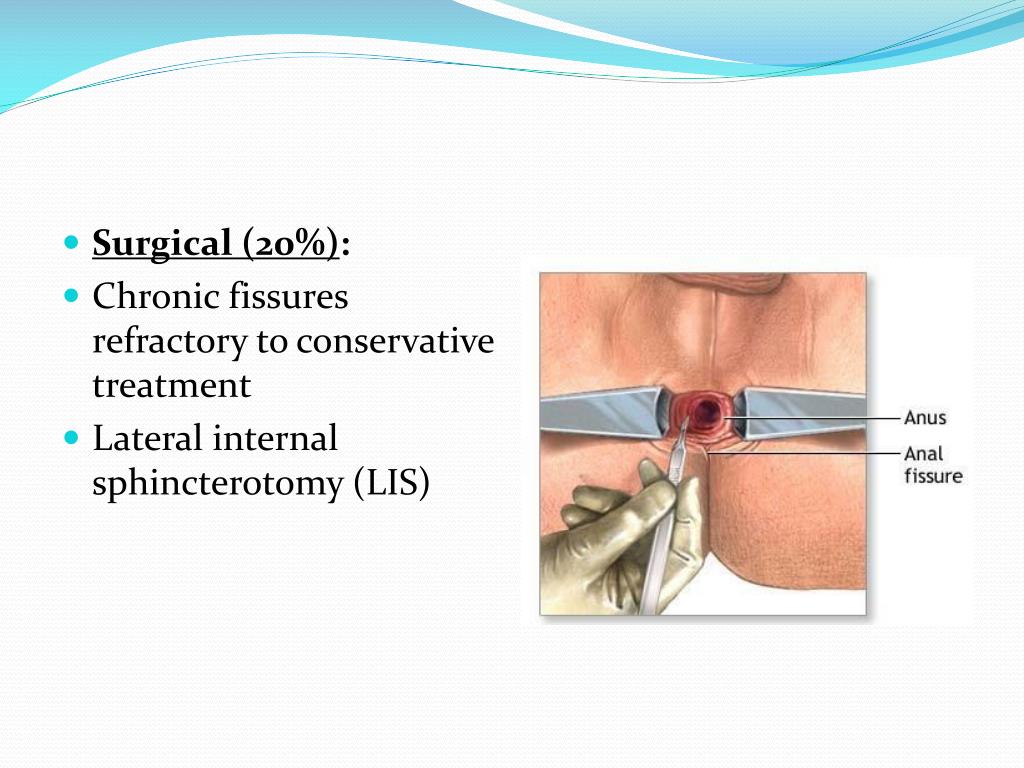
These practices heal most fissures (80 to 90 percent) within several weeks to several months. However, when treatments fail and anal fissures persist or come back, other measures can be tried, including:
Before surgery is considered, your doctor will re-examine you and may conduct other tests to determine why other treatments have failed to heal the fissure.
A fissure may fail to heal because of scarring or muscle spasms of the internal anal sphincter muscle. Surgery usually consists of making a cut to a small portion of the internal anal sphincter muscle to reduce pain and spasms and allow the fissure to heal. Cutting the muscle rarely results in the loss of ability to control bowel movements.
The surgery can usually be performed on an outpatient basis (the patient goes home the same day). Pain is relieved after a few days and complete healing takes place in a few weeks.
Last reviewed by a Cleveland Clinic medical professional on 02/22/2019.
American Society of Colon and Rectal Surgeons. Anal Fissure. Accessed 2/22/2019.
American Pediatric Surgical Association. Anal Fissure. Accessed 2/22/2019.
Sugerman DT. Anal Fissure. JAMA. 2014;311(11):1171. doi:10.1001/jama.2014.214
Get useful, helpful and relevant health + wellness information
Find the latest information from the globally recognized leader in digestive diagnosis, treatments and surgical innovations.
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
9500 Euclid Avenue, Cleveland, Ohio 44195 | 800.223.2273 | © 2021 Cleveland Clinic. All Rights Reserved.
WebMD processes personal data about users of our site, including health data, through the use of cookies to deliver our services, personalize advertising and to analyze site activity. We may share certain information about our users with our advertising and analytics partners. For additional details, refer to the WebMD Privacy Policy and WebMD Cookie Policy.
By clicking "I AGREE" below, you agree to the WebMD Privacy Policy and WebMD Cookie Policy and WebMD’s personal data processing and cookie practices as described therein.
© 1996-2021 MedicineNet, Inc. All rights reserved. Terms of Use.
MedicineNet does not provide medical advice, diagnosis or treatment. See additional information.
What should I know about anal fissures?
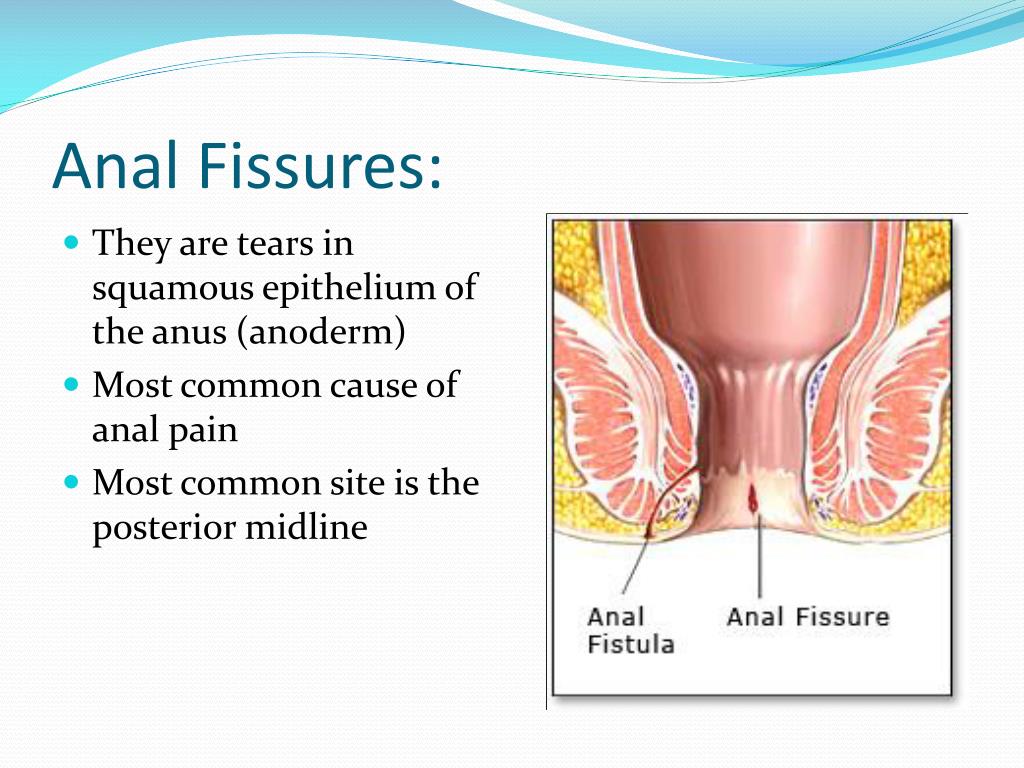
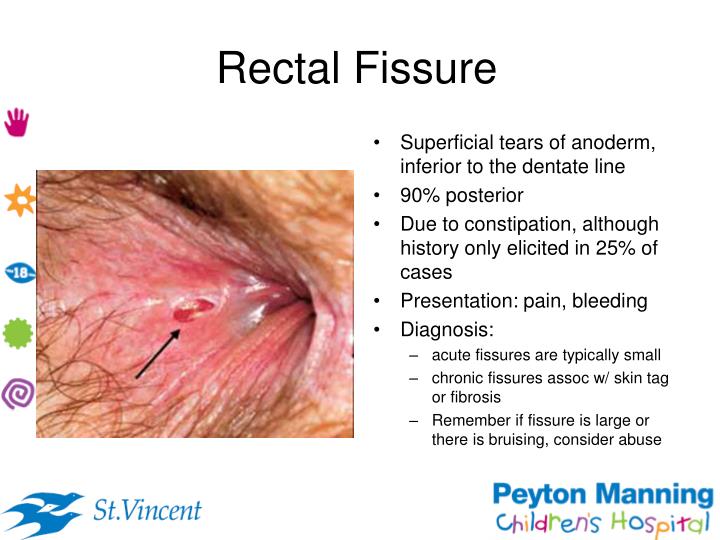
An anal fissure is a cut or tear occurring in the anus (the opening through which stool passes out of the body) that extends upwards into the anal canal. Fissures are a common condition of the anus and anal canal and are responsible for 6% to 15% of the visits to a colon and rectal (colorectal) surgeon. They affect men and women equally and both the young and the old. Fissures usually cause pain during bowel movements that often is severe. Anal fissure is the most common cause of rectal bleeding in infancy.
Anal fissures occur in the specialized tissue that lines the anus and anal canal, called anoderm. At a line just inside the anus (referred to as the anal verge or intersphincteric groove) the skin (dermis) of the inner buttocks changes to anoderm. Unlike skin, anoderm has no hairs, sweat glands, or sebaceous (oil) glands and contains a larger number of sensory nerves that sense light touch and pain. (The abundance of nerves explains why anal fissures are so painful.) The hairless, gland-less, extremely sensitive anoderm continues for the entire length of the anal canal until it meets the demarcating line for the rectum, called the dentate line. (The rectum is the distal 15 cm of the colon that lies just above the anal canal and just below the sigmoid colon.)
Anal fissures are caused primarily by trauma, but several non-traumatic diseases are associated with anal fissures and should be suspected if fissures occur in unusual locations.
Anal fissures are diagnosed and evaluated by visual inspection of the anus and anal canal.
Anal fissures are initially treated conservatively with home remedies and OTC products that include adding bulk to the stool, softening the stool, consuming a high fiber diet, and utilizing sitz baths.
Prescription drugs used to treat anal fissures that fail to heal with less conservative treatment are ointments containing anesthetics, steroids, nitroglycerin, and calcium channel blocking drugs (CCBs).
Surgery by lateral sphincterotomy is the gold standard for curing anal fissures. Because of complications, however, it is reserved for patients who are intolerant of non-surgical treatments or in whom non-surgical treatments have proven to be ineffective.
What are the signs and symptoms of anal fissures?
People with anal fissures almost always experience anal pain that worsens with bowel movements.
As previously mentioned, anal fissures commonly bleed in infants.
Anal fissures are caused by trauma to the anus and anal canal. The cause of the trauma usually is a bowel movement, and many people can remember the exact bowel movement during which their pain began. The fissure may be caused by a hard stool or repeated episodes of diarrhea. Occasionally, the insertion of a rectal thermometer, enema tip, endoscope, or ultrasound probe (for examining the prostate gland) can result in sufficient trauma to produce a fissure. During childbirth, trauma to the perineum (the skin between the posterior vagina and the anus) may cause a tear that extends into the anoderm.
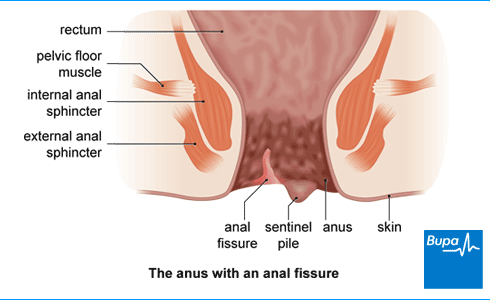
The most common location for an anal fissure in both men and women (90% of all fissures) is the midline posteriorly in the anal canal, the part of the anus nearest the spine. Fissures are more common posteriorly because of the configuration of the muscle that surrounds the anus. This muscle complex, referred to as the external and internal anal sphincters, underlies and supports the anal canal. The sphincters are oval-shaped and are best supported at their sides and weakest posteriorly. When tears occur in the anoderm, therefore, they are more likely to be posterior. In women, there also is weak support for the anterior anal canal due to the presence of the vagina anterior to the anus. For this reason, 10% of fissures in women are anterior, while only 1% are anterior in men. At the lower end of fissures a tag of skin may form, called a sentinel pile.
When fissures occur in locations other than the midline posteriorly or anteriorly, they should raise the suspicion that a problem other than trauma is the cause. Other causes of fissures are anal cancer, Crohn's disease, leukemia as well as many infectious diseases including tuberculosis, viral infections (cytomegalovirus or herpes), syphilis, gonorrhea, Chlamydia , chancroid (Hemophilus ducreyi), and human immunodeficiency virus (HIV). Among patients with Crohn's disease, 4% will have an anal fissure as the first manifestation of their Crohn's disease, and half of all patients with Crohn's disease eventually will develop an anal ulceration that may look like a fissure.
Studies of the anal canal in patients with anal fissures consistently show that the muscles surrounding the anal canal are contracting too strongly (they are in spasm), thereby generating a pressure in the canal that is abnormally high. The two muscles that surround the anal canal are the external anal sphincter and the internal anal sphincter (already discussed). The external anal sphincter is a voluntary (striated) muscle, that is, it can be controlled consciously. Thus, when we need to have a bowel movement we can either tighten the external sphincter and prevent the bowel movement, or we can relax it and allow the bowel movement. On the other hand, the internal anal sphincter is an involuntary (smooth) muscle, that is, a muscle we cannot control. The internal sphincter is constantly contracted and normally prevents small amounts of stool from leaking from the rectum. When a substantial load of stool reaches the rectum, as it does just prior to a bowel movement, the internal anal sphincter relaxes automatically to let the stool pass (that is, unless the external anal sphincter is consciously tightened).
When an anal fissure is present, the internal anal sphincter is in spasm. In addition, after the sphincter finally does relax to allow a bowel movement to pass, instead of going back to its resting level of contraction and pressure, the internal anal sphincter contracts even more vigorously for a few seconds before it goes back to its elevated resting level of contraction. It is thought that the high resting pressure and the "overshoot" contraction of the internal anal sphincter following a bowel movement pull the edges of the fissure apart and prevent the fissure from healing.
The supply of blood to the anus and anal canal also may play a role in the poor healing of anal fissures. Anatomic and microscopic studies of the anal canal on cadavers found that in 85% of individuals that the posterior part of the anal canal (where most fissures occur) has less blood flowing to it than the other parts of the anal canal. Moreover, ultrasound studies that measure the flow of blood showed that the posterior anal canal had less than half of the blood flow of other parts of the canal. This relatively poor flow of blood may be a factor in preventing fissures from healing. It also is possible that the increased pressure in the anal canal due to spasm of the internal anal sphincter may compress the blood vessels of the anal canal and further reduce the flow of blood.
What exams, procedures, and tests diagnose anal fissures?
A careful history usually suggests that an anal fissure is present, and gentle inspection of the anus can confirm the presence of a fissure. If gentle eversion (pulling apart) the edges of the anus by separating the buttocks does not reveal a fissure, a more vigorous examination following the application of a topical anesthetic to the anus and anal canal may be necessary. A cotton-tipped swab may be inserted into the anus to gently localize the source of the pain.
An acute anal fissure looks like a linear tear. A chronic anal fissure frequently is associated with a triad of findings that includes a tag of skin at the edge of the anus (sentinel pile), thickened edges of the fissure with muscle fibers of the internal sphincter visible at the base of the fissure, and an enlarged anal papilla at the upper end of the fissure in the anal canal.
If rectal bleeding is present, an endoscopic evaluation using a rigid or flexible viewing tube is necessary to exclude the possibility of a more serious disease of the anus and rectum. A sigmoidoscopy that examines only the distal part of the colon may be reasonable in patients younger than 50 years of age who have a typical anal fissure. In patients with a family history of colon cancer or age greater than 50 (and, therefore, at higher risk for colon cancer), a colonoscopy that examines the entire colon is recommended. Atypical fissures that suggest the presence of other diseases, as discussed previously, require other diagnostic studies including colonoscopy and upper gastrointestinal (UGI) and small intestinal X-rays.
What home remedies and over-the-counter drugs treat anal fissures?
The goal of treatment for anal fissures is to break the cycle of spasm of the anal sphincter and its repeated tearing of the anoderm. In acute fissures, medical (nonoperative) therapy is successful in the majority of patients. Of acute fissures, 80% to 90% will heal with conservative measures as compared with chronic (recurrent) fissures, which show only a 40% rate of healing. Initial treatment involves adding bulk to the stool and softening the stool with psyllium or methylcellulose preparations and a high fiber diet.
Other home remedies for anal fisures include avoiding "sharp" foods that may not be well-digested (i.e., nuts, popcorn, tortilla chips); increase liquid intake, and, at times, take stool softeners (docusate or mineral oil preparations). Sitz baths (essentially soaking in a tub of warm water). Sitz baths are encouraged, particularly after bowel movements, to relax the spasm, to increase the flow of blood to the anus, and to clean the anus without rubbing the irritated anoderm.
The author has found that when there are enlarged internal hemorrhoids in addition to a fissure, that healing of the fissure is improved if the hemorrhoids are treated with sclerotherapy that shrinks them. After application of a topical anesthetic, if a patient can tolerate a gentle examination of the rectum with a finger and an anoscope can be inserted through the anus, enlarged hemorrhoids can be identified, and if present, treated with sclerotherapy. (It is unclear if improvement in healing is caused by anal dilation with the finger or by shrinkage of the hemorrhoid.)
What prescription drugs treat anal fissures?
Topical anesthetics (for example, xylocaine, lidocaine, tetracaine, pramoxine) are recommended especially prior to a bowel movement to reduce the pain of defecation. Often, a small amount of a steroid is combined in the anesthetic cream to reduce inflammation. The use of steroids should be limited to two weeks because longer use will result in thinning of the anoderm (atrophy), which makes it more susceptible to trauma. Oral medications to relax the smooth muscle of the internal sphincter have not been shown to aid healing.
Because of the possibility that spasm of the internal sphincter and reduced flow of blood to the sphincter play roles in the formation and healing of anal fissures, ointments with the muscle relaxant, nitroglycerin (glyceryl trinitrate), have been tried and found to be effective in healing anal fissures. Glycerin trinitrate (nitroglycerin) has been shown to cause relaxation of the internal anal sphincter and to decrease the anal resting pressure. When ointments containing nitroglycerin are applied to the anal canal, the nitroglycerin diffuses across the anoderm and relaxes the internal sphincter and reduces the pressure in the anal canal. This relieves spasm of the muscle and also may increase the flow of blood, both of which promote healing of fissures. Unlike Nitropaste, a 2.0% concentration of nitroglycerin that is used on the skin for patients with heart disease and angina, the nitroglycerin ointment used for treating anal fissures contains a concentration of nitroglycerin of only 0.2%. One randomized, controlled trial has demonstrated the healing of anal fissures in 68% of patients with nitroglycerin as compared to 8% of patients treated with placebo (inactive treatment). Other studies have shown a 33% to 47% recurrence rate of fissures following treatment with nitroglycerin. The presence of a sentinel pile is associated with a lower healing rate with nitroglycerin treatment.
The dose of nitroglycerin often is limited by side effects. The usual side effects are headache (due to dilation of blood vessels in the head) or light-headedness (due to a drop in blood pressure). This author recommends that a small amount of ointment be applied to a cotton-tipped swab with the swab then inserted into the anus only for the depth of the cotton-tipped portion of the swab. Ointment smeared only around the outside of the anus does not reach the anoderm where its effects are important, yet the nitroglycerin will be absorbed and produce side effects.
Nitroglycerin is more rapidly absorbed if blood flow in the anoderm is high. For this reason, it is recommended that nitroglycerin not be applied within 30 minutes of a bath since the warm water of the bath enlarges (dilates) the blood vessels in the skin and anoderm and increases their flow of blood. Additionally, the first application of nitroglycerin should be at bedtime while the patient is lying down in order to prevent falls due to light-headedness.
The side effects of nitroglycerin often are self-limited, that is, they become less with repeated use. Caffeine can help reduce or prevent headaches. However, if side effects are pronounced, nitroglycerin should be discontinued. Drugs for impotence (for example, sildenafil (Viagra), should not be used together with nitroglycerin since they increase the risk of developing low blood pressure.
As is the case with nitroglycerin, ointments containing calcium channel blocking drugs (for example, nifedipine [Adalat] or diltiazem [Cardizem]) relax the muscles of the internal sphincter. They also expand the blood vessels of the anoderm and increase the flow of blood. Nifedipine ointment (2%) is applied in a manner similar to nitroglycerin ointment, but seems to produce fewer side effects
12 Year Teen Fucking
Asanas Ass Xxx
Xxx Video Bbw And Negr
Alexis Texas Sex Videos
Curvy Teen Boobs
Anal fissure - Symptoms and causes - Mayo Clinic
Anal Fissures: Causes, Symptoms, Treatment & Prevention
Anal Fissure: Treatment, Symptoms, Natural Remedies ...
Anal Pain: Causes, Diagnosis & Treatment
Common Causes of Rectal and Anal Pain - Verywell Health
Anal pain - Mayo Clinic
Rectal Pain: 16 Causes in Men, Women, Other Symptoms
Anal Pain Causes and Treatment Guide - Verywell Health
9 Rectal Pain Causes, Symptoms and Relief Options | Buoy
Tears Anal Pain












(mh%3dufNrfuQ-o_PpfQSR)1.jpg)