Sperm Extraction
⚡ ALL INFORMATION CLICK HERE 👈🏻👈🏻👈🏻
Sperm Extraction
Войдите в аккаунт, чтобы подтвердить свой возраст.
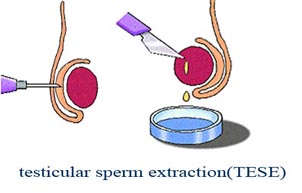
Testicular sperm extraction (TESE)
Microscopic Testicular Sperm Extraction by Dr. Manu Gupta - YouTube
Testicular sperm extraction — Wikipedia Republished // WIKI 2
Sperm Extraction смотреть видео онлайн в hd качестве 1080
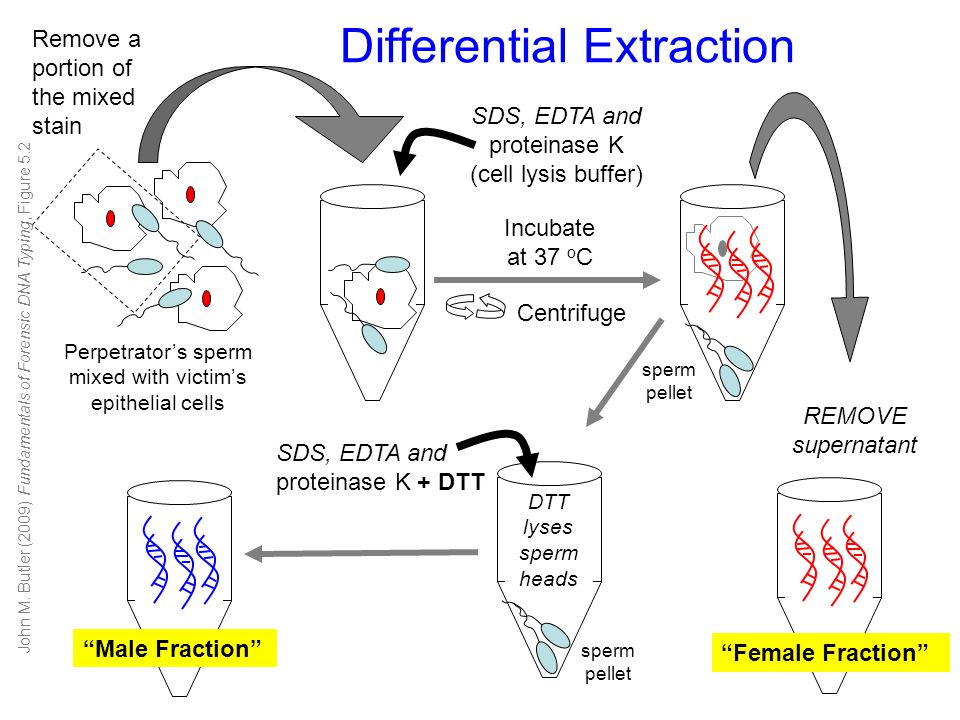
(PDF) Genomic DNA Extraction from Sperm
Tissue is extracted from the seminiferous tubules during surgery in TESE
^ Graham, Sam D.; Keane, Thomas E. (2015-09-04). Glenn's urologic surgery . Keane, Thomas E.,, Graham, Sam D., Jr.,, Goldstein, Marc (8th ed.). Philadelphia, PA. ISBN 9781496320773 . OCLC 927100060 .
^ a b c Dabaja, Ali A.; Schlegel, Peter N. (2013). "Microdissection testicular sperm extraction: an update" . Asian Journal of Andrology . 15 (1): 35–39. doi : 10.1038/aja.2012.141 . ISSN 1745-7262 . PMC 3739122 . PMID 23241638 .
^ a b Flannigan, Ryan; Bach, Phil V.; Schlegel, Peter N. (2017). "Microdissection testicular sperm extraction" . Translational Andrology and Urology . 6 (4): 745–752. doi : 10.21037/tau.2017.07.07 . ISSN 2223-4691 . PMC 5583061 . PMID 28904907 .
^ Gies, Inge; Oates, Robert; De Schepper, Jean; Tournaye, Herman (2016). "Testicular biopsy and cryopreservation for fertility preservation of prepubertal boys with Klinefelter syndrome: a pro/con debate" . Fertility and Sterility . 105 (2): 249–255. doi : 10.1016/j.fertnstert.2015.12.011 . ISSN 1556-5653 . PMID 26748226 .
^ "Infertility - Treatment" . nhs.uk . 2017-10-23 . Retrieved 2019-09-24 .
^ Liu, Wen; Schulster, Michael L.; Alukal, Joseph P.; Najari, Bobby B. (2019-08-16). "Fertility Preservation in Male to Female Transgender Patients". Urologic Clinics of North America . 46 (4): 487–493. doi : 10.1016/j.ucl.2019.07.003 . ISSN 0094-0143 . PMID 31582023 .
^ a b c Esteves, Sandro C.; Miyaoka, Ricardo; Agarwal, Ashok (2011). "Sperm retrieval techniques for assisted reproduction" . International Braz J Urol . 37 (5): 570–583. doi : 10.1590/s1677-55382011000500002 . ISSN 1677-6119 . PMID 22099268 .
^ "Surgical sperm extraction | Human Fertilisation and Embryology Authority" . www.hfea.gov.uk . Retrieved 2019-09-25 .
^ a b c Janosek-Albright, Kirsten J. C.; Schlegel, Peter N.; Dabaja, Ali A. (2015). "Testis sperm extraction" . Asian Journal of Urology . 2 (2): 79–84. doi : 10.1016/j.ajur.2015.04.018 . ISSN 2214-3882 . PMC 5730746 . PMID 29264124 .
^ a b "What is Sperm Retrieval? - Urology Care Foundation" . www.urologyhealth.org . Retrieved 2019-09-24 .
^ a b c Tsujimura, Akira (2007). "Microdissection testicular sperm extraction: prediction, outcome, and complications". International Journal of Urology . 14 (10): 883–889. doi : 10.1111/j.1442-2042.2007.01828.x . ISSN 0919-8172 . PMID 17880285 .
^ a b Bernie, Aaron M.; Mata, Douglas A.; Ramasamy, Ranjith; Schlegel, Peter N. (2015). "Comparison of microdissection testicular sperm extraction, conventional testicular sperm extraction, and testicular sperm aspiration for nonobstructive azoospermia: a systematic review and meta-analysis". Fertility and Sterility . 104 (5): 1099–1103.e1–3. doi : 10.1016/j.fertnstert.2015.07.1136 . ISSN 1556-5653 . PMID 26263080 .
^ Klami, Rauni; Mankonen, Harri; Perheentupa, Antti (2018). "Successful microdissection testicular sperm extraction for men with non-obstructive azoospermia". Reproductive Biology . 18 (2): 137–142. doi : 10.1016/j.repbio.2018.03.003 . ISSN 2300-732X . PMID 29602610 .
^ Chiba, Koji; Enatsu, Noritoshi; Fujisawa, Masato (2016). "Management of non-obstructive azoospermia" . Reproductive Medicine and Biology . 15 (3): 165–173. doi : 10.1007/s12522-016-0234-z . ISSN 1445-5781 . PMC 5715857 . PMID 29259433 .
^ "Surgical sperm extraction | Human Fertilisation and Embryology Authority" . www.hfea.gov.uk . Retrieved 2019-09-24 .
^ "Microscopic Testicular Sperm Extraction + Fertility" . Cleveland Clinic . Retrieved 2019-09-24 .
This page was last edited on 17 April 2020, at 10:54
Basis of this page is in Wikipedia . Text is available under the CC BY-SA 3.0 Unported License . Non-text media are available under their specified licenses. Wikipedia® is a registered trademark of the Wikimedia Foundation, Inc. WIKI 2 is an independent company and has no affiliation with Wikimedia Foundation.
To install click the Add extension button. That's it.
The source code for the WIKI 2 extension is being checked by specialists of the Mozilla Foundation, Google, and Apple. You could also do it yourself at any point in time.
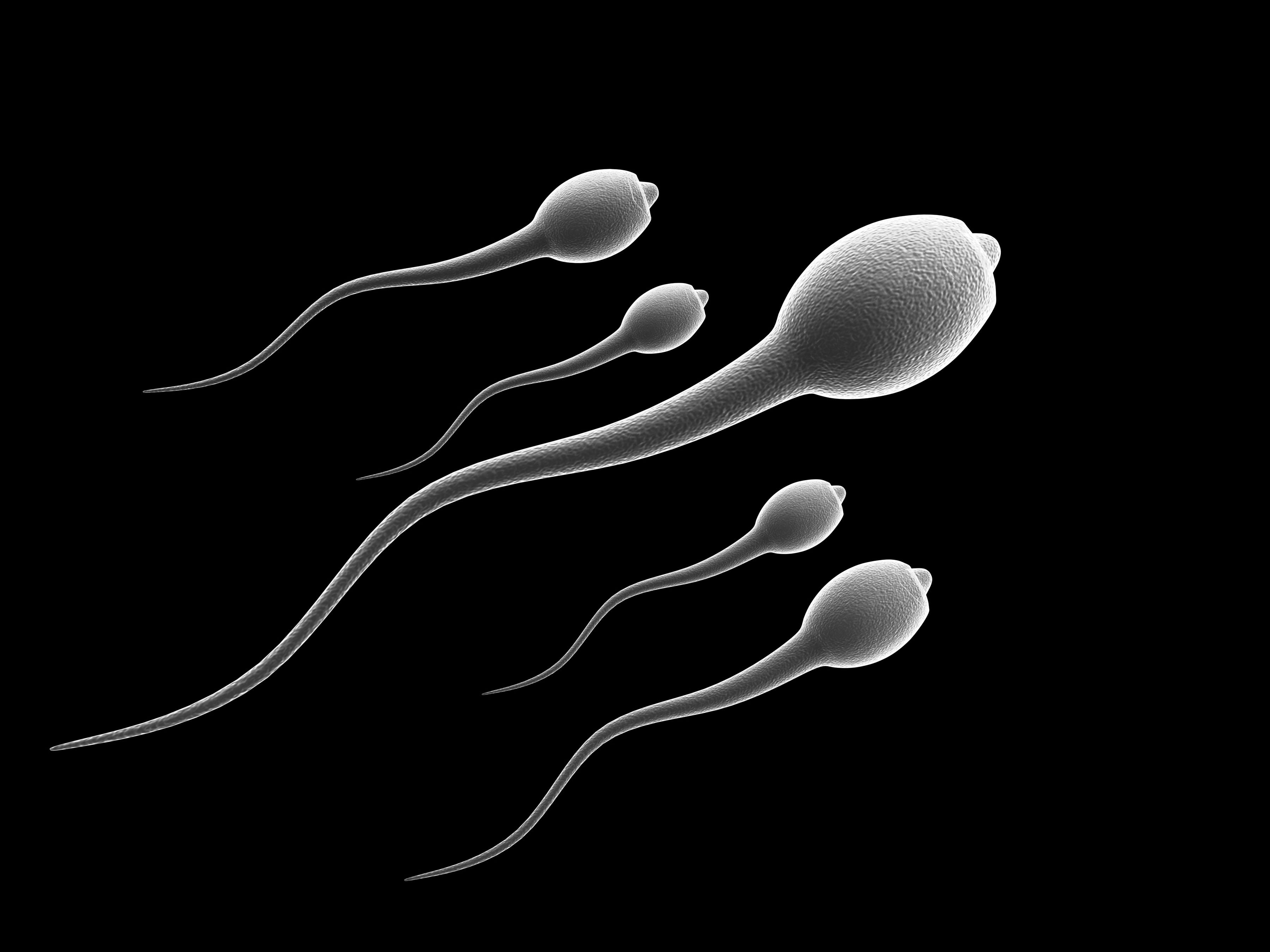
Testicular sperm extraction (TESE) is the surgical procedure of removing a small portion of tissue from the testicle and extracting any viable sperm cells from that tissue for use in further procedures, most commonly intracytoplasmic sperm injection (ICSI) as part of in vitro fertilisation (IVF). [1] TESE is often recommended to patients who cannot produce sperm by ejaculation due to azoospermia . [2]
TESE is recommended to patients who do not have sperm present in their ejaculate, azoospermia, or who cannot ejaculate at all. In general, azoospermia can be divided into obstructive and non-obstructive subcategories.
TESE is primarily used for non-obstructive azoospermia, where patients do not have sperm present in the ejaculate but who may produce sperm in the testis. Azoospermia in these patients could be a result of Y chromosome microdeletions , cancer of the testicles or damage to the pituitary gland or hypothalamus , which regulate sperm production. Often in these cases, TESE is used as a second option, after prior efforts to treat the azoospermia through hormone therapy have failed. [3]
However, if azoospermia is related to a disorder of sexual development , such as Klinefelter syndrome , TESE is not currently used clinically; this is currently in the research phase. [4]
More rarely, TESE is used to extract sperm in cases of obstructive azoospermia. Obstructive azoospermia can be caused in a variety of ways:
TESE can also be used as a fertility preservation option for patients undergoing gender reassignment surgery and who cannot ejaculate sperm. [6]
Conventional TESE is usually performed under local, or sometimes spinal or general, anaesthesia . [7] [8] An incision in the median raphe of the scrotum is made and continued through the dartos fibres and the tunica vaginalis. The testicle and epidydymis are then visible. [9] From here incision/s are through the outer covering of the testis to retrieve biopsies of seminiferous tubules, the structures which contain sperm. The incision is closed with sutures and each sample is assessed under a microscope to confirm the presence of sperm. [7]
Following extraction, sperm is often cryogenically preserved for future use, but can also be used fresh. [10]
Micro-TESE, or microdissection testicular sperm extraction, includes the use of an operating microscope . This allows the surgeon to observe regions of seminiferous tubules of the testes that have more chance of containing spermatozoa. [2] The procedure is more invasive than conventional TESE, requiring general anaesthetic, and usually used only in patients with non-obstructive azoospermia. [11] Similarly to TESE, an incision is made in the scrotum and surface of the testicle to expose seminiferous tubules. However, this exposure is much more wide in micro-TESE. This allows exploration of the incision under the microscope to identify areas of tubules more likely to contain more sperm. If none can be identified, biopsies are instead taken at random from a wide range of locations. The incision is closed with sutures. Samples are re-examined post-surgery to locate and then purify sperm. [7]
When compared with conventional TESE, micro-TESE generally has higher success in extracting sperm; as such, micro-TESE is preferable in cases of non-obstructive azoospermia, where infertility is caused by a lack of sperm production rather than a blockage. [12] [10] In these cases, micro-TESE is more likely to yield sufficient sperm for use in ICSI. [13]
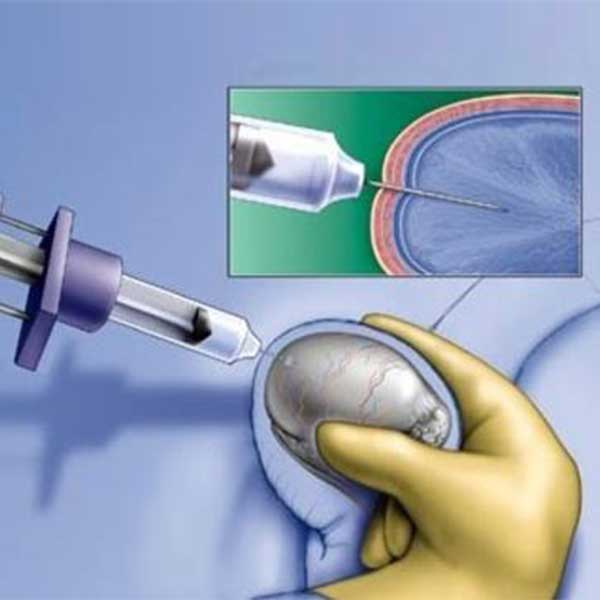
TESE is different to testicular sperm aspiration (TESA). TESA is done under local anaethesia, does not involve an open biopsy and is suitable for patients with obstructive azoospermia. [12]
Like all surgical operations, micro-TESE and TESE have risks of postoperative infection, bleeding and pain. [9] However, TESE can result in testicular abnormalities and scarring of the tissue. The procedure can also cause testicular fibrosis and inflammation, which can reduce testicular function and cause testicular atrophy. [14] Both procedures can alter the steroid function of the testes causing a decline in serum testosterone levels, which can result in testosterone deficiency . [11] This can cause side-effects including muscle weakness, decreased sexual function, anxiety, leading to sleep deficiency. [15] The blood supply to the testis can also be altered during this procedure, potentially reducing supply. Long-term follow-ups are often recommended to prevent these complications. [11]
Micro-TESE has limited postoperative complications compared with TESE. The use of the surgical microscope allows for small specific incisions to retrieve seminiferous tubules and evade damaging blood vessels by avoiding regions with no vasculature. [3] [9]
If TESE needs to be repeated due to insufficient sperm recovery, patients are usually advised to wait 6–12 months in order to allow adequate healing of the testis before further surgery. [16]
Sensual Sex Massage
Reality Kings Party
Cindy Sheri Vi Oral Sex Pre
Big Dick Anal Penetration
Hd Girls Solo Tit


















_V0.1_JB.png)