Sperm Analysis

⚡ ALL INFORMATION CLICK HERE 👈🏻👈🏻👈🏻
Sperm Analysis
Share on Pinterest A sperm analysis can help a doctor diagnose fertility problems.
Share on Pinterest A sperm analysis can help identify issues with sperm count, motility, or shape.
Share on Pinterest A doctor may recommend further tests to identify the cause of abnormal results.
Medically reviewed by J. Keith Fisher, M.D. — Written by Jayne Leonard on November 19, 2018
Medically reviewed by Emelia Arquilla, DO
Medically reviewed by Daniel Murrell, MD
© 2004-2021 Healthline Media UK Ltd, Brighton, UK, a Red Ventures Company. All rights reserved. MNT is the registered trade mark of Healthline Media. Any medical information published on this website is not intended as a substitute for informed medical advice and you should not take any action before consulting with a healthcare professional
A sperm analysis involves checking a sample of semen for overall sperm health.
The process can help doctors to determine the underlying cause of a person’s inability to conceive, or it may confirm the outcome of a vasectomy.
A sperm analysis tests for several markers of sperm health, including:
In this article, we describe the purpose and procedure involved in sperm analysis, and we explain what the results may mean.
People may require a sperm analysis for different reasons. Some individuals or couples will request a sperm analysis if they are having difficulty conceiving.
In couples that have been unable to conceive, some estimates suggest that there is a male factor present in 40 to 50 percent of cases.
Up to 2 percent of men demonstrate issues with their sperm, resulting from one or a combination of:
People may also have a sperm analysis to check if a vasectomy was successful. A vasectomy is a surgical procedure that doctors carry out for permanent male sterilization.
Following a vasectomy, doctors typically recommend regular sperm analyses for several months to ensure there are no sperm remaining in the semen.
Usually, a doctor will require a person to provide a semen sample while in the doctor’s office.
The most common way to collect a sample is for a person to masturbate and ejaculate into a sterile cup. The doctor provides a private room for a person to do this.
In some cases, a person can collect the semen sample at home. A doctor can provide a special condom that allows a person to collect a semen sample during sexual activity.
Otherwise, a doctor may recommend that the person ejaculates into a collection cup while at home.
When collecting a sample at home, people must remember to keep it at room temperature and bring it to the laboratory within a short timescale after collection.
To make sure that the sample is usable, the doctor may require that a person:
The American Association for Clinical Chemistry recommends that medical professionals carry out 2 or more separate sperm analyses within 2- to 3-week intervals.
As sperm profiles can vary from day-to-day, an average of these results may give the most accurate picture of sperm health.
The results of a sperm analysis should be ready within a few days.
A sperm analysis looks at several factors when considering the health of the sperm. We discuss these factors and their results below.
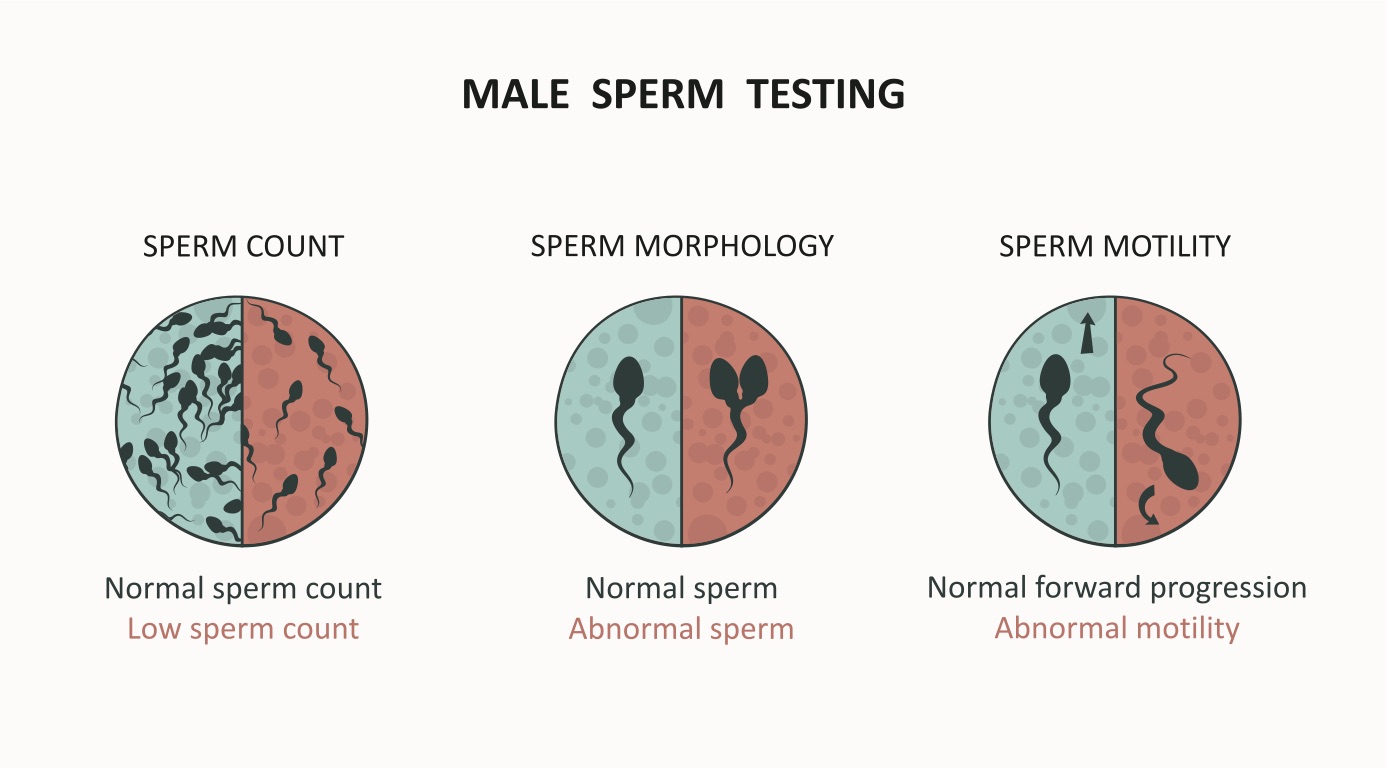
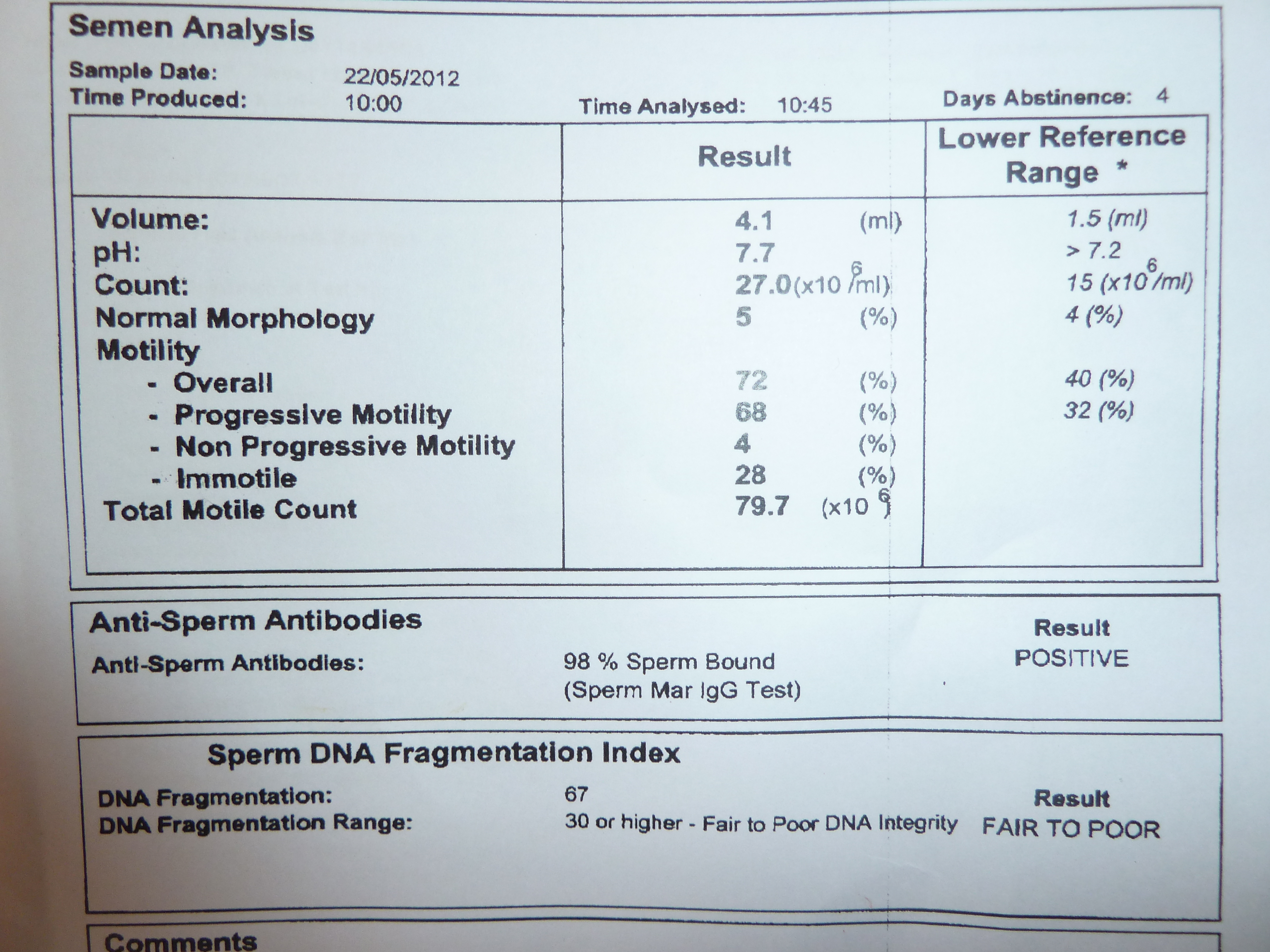
Sperm count refers to the number of sperm that are present in 1 ml of semen. World Health Organization (WHO) guidelines suggest that a normal sperm count is at least 15 million per ml or no fewer than 39 million sperm per sample.
Having less than this indicates a low sperm count. Some research suggests that up to 90 percent of male infertility issues result from abnormal sperm counts.
Home sperm analysis kits usually only test for sperm count. As this is just one aspect of male fertility, it is important that people see their doctor and get comprehensive sperm analysis to check for other factors affecting their sperm.
Sperm motility is the ability of the sperm to move efficiently. Low motility can reduce the sperm’s capacity to move through the female reproductive system to fertilize the egg.
In a typical sample, at least 50 percent of the sperm will demonstrate normal motility.
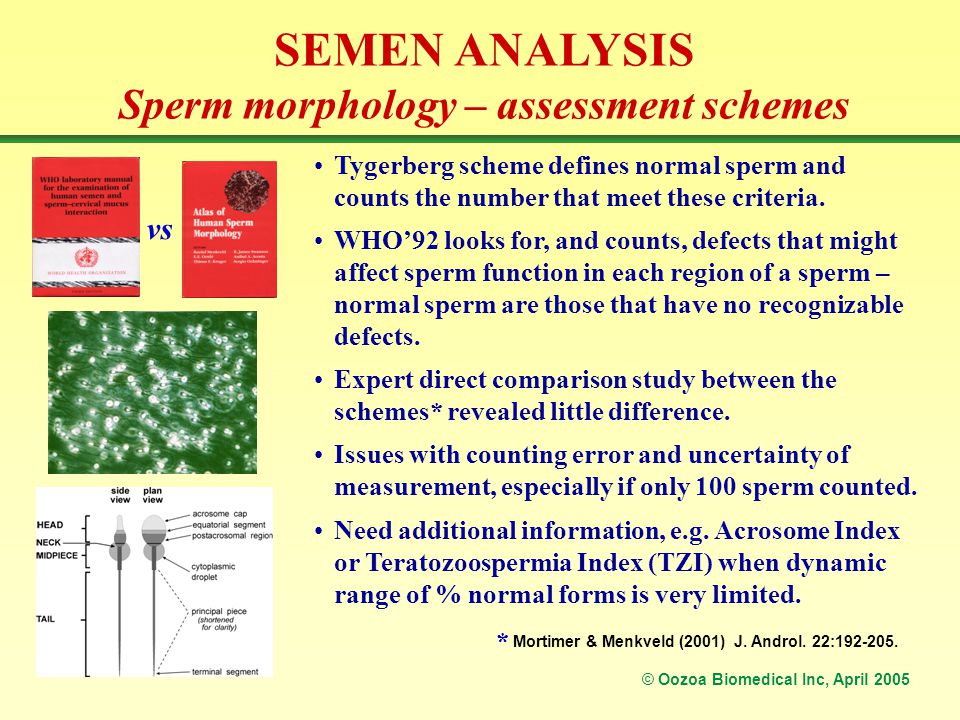
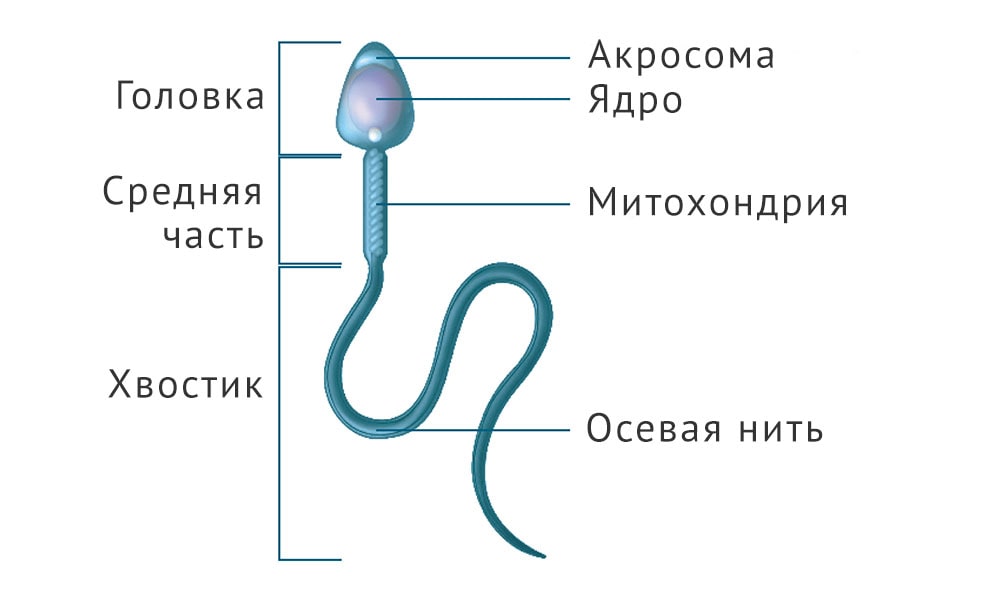
Morphology refers to the size and the shape of the individual sperm. Normal sperm have a long tail and oval-shaped head. Abnormally sized or shaped sperm can have difficulty reaching, penetrating, and fertilizing the egg.
Normal semen contains a minimum of 4 percent sperm with standard form.
Although sperm count, motility, and morphology are three of the main factors that medical professionals will check when assessing male fertility, they are not the only factors.
Other factors that doctors consider when doing a sperm analysis include:
The Centers for Disease Control and Prevention (CDC) advise that a slightly abnormal sperm analysis does not mean that a person is permanently infertile. Instead, doctors can use the results as a tool to help identify what factors are causing fertility issues.
People who receive abnormal results from a semen analysis typically undergo further testing to help identify the exact issue. In many cases, a person’s fertility issues resolve with the right treatment.
Following a vasectomy, doctors will check a person’s semen for the presence of sperm.
If the semen sample does not contain any sperm, people may be able to stop using condoms and other forms of birth control , as pregnancy is unlikely.
However, if sperm is still present, people should continue using contraceptives to prevent unwanted pregnancies. They may need further sperm analysis tests until their semen no longer shows the presence of sperm.
A sperm analysis is one of the first tests that males undergo to look for the reasons for difficulty with conceiving. People also require sperm analysis to check the success of a vasectomy.
If sperm analysis results are abnormal, a doctor will typically recommend further testing to help find the underlying cause and formulate a treatment plan.
Many cases of male infertility are treatable with lifestyle changes, medications, surgery, and other interventions. If these are unsuccessful, a doctor or fertility counselor can help people explore other options, such as donor sperm or adoption.
Last medically reviewed on November 19, 2018
Semen Analysis : Sperm Count Test Procedure and Results
Sperm (semen) analysis : Uses, procedure, and results
Semen Analysis ( Sperm Count Testing) | HealthEngine Blog
Sperm analysis | Sperm under a microscope | Competently about health on...
Sperm Analysis Results: What Do They Mean and How To Get Help
Health Topics
Cold & Flu
Dental Care
Back Pain
Eye Care
Mental Health
Ear, Nose, Throat
Skincare and Beauty
Pregnancy
HealthEngine
Contact Us
About Us
About Authors
Practice Services
Blog
List a Practice
List Your Appointments
Find a Practice
Find a Practitioner
GP Appointments
After Hours GP Appointments
Bulk Billing GP Appointments
Dentist Appointments Near You
Physiotherapist Appointments
Chiropractor Appointments
Psychologist Appointments
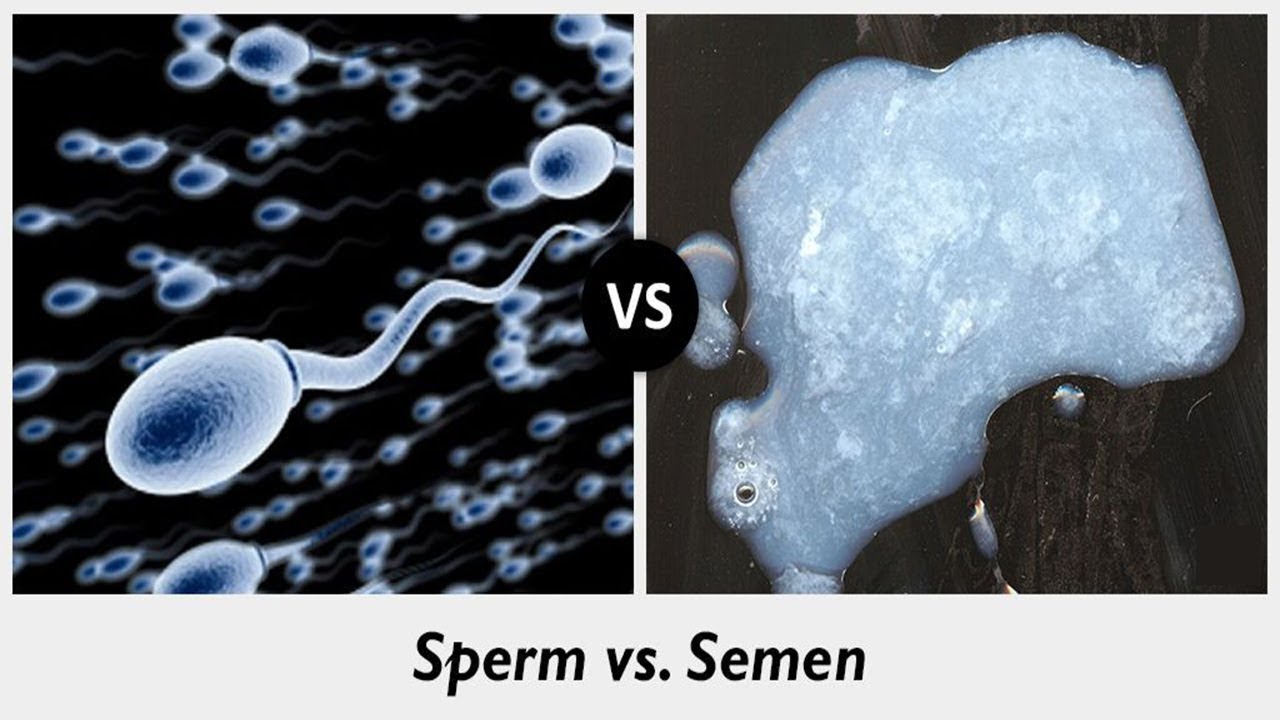
Sperm is the male gamete , that is, the male sex cell , or the cell in males which has the capacity to fertilise an egg (i.e. a female gamete, also known as an ovum or oocyte). Sperm are produced in the seminiferous tubes of the testes .
The pituitary gland at the base of the brain causes testosterone to be produced in the testes. Testerosterone causes sperms to be produced. The sperm production cycle takes approximately three months and a healthy man produces millions of new sperm each day.
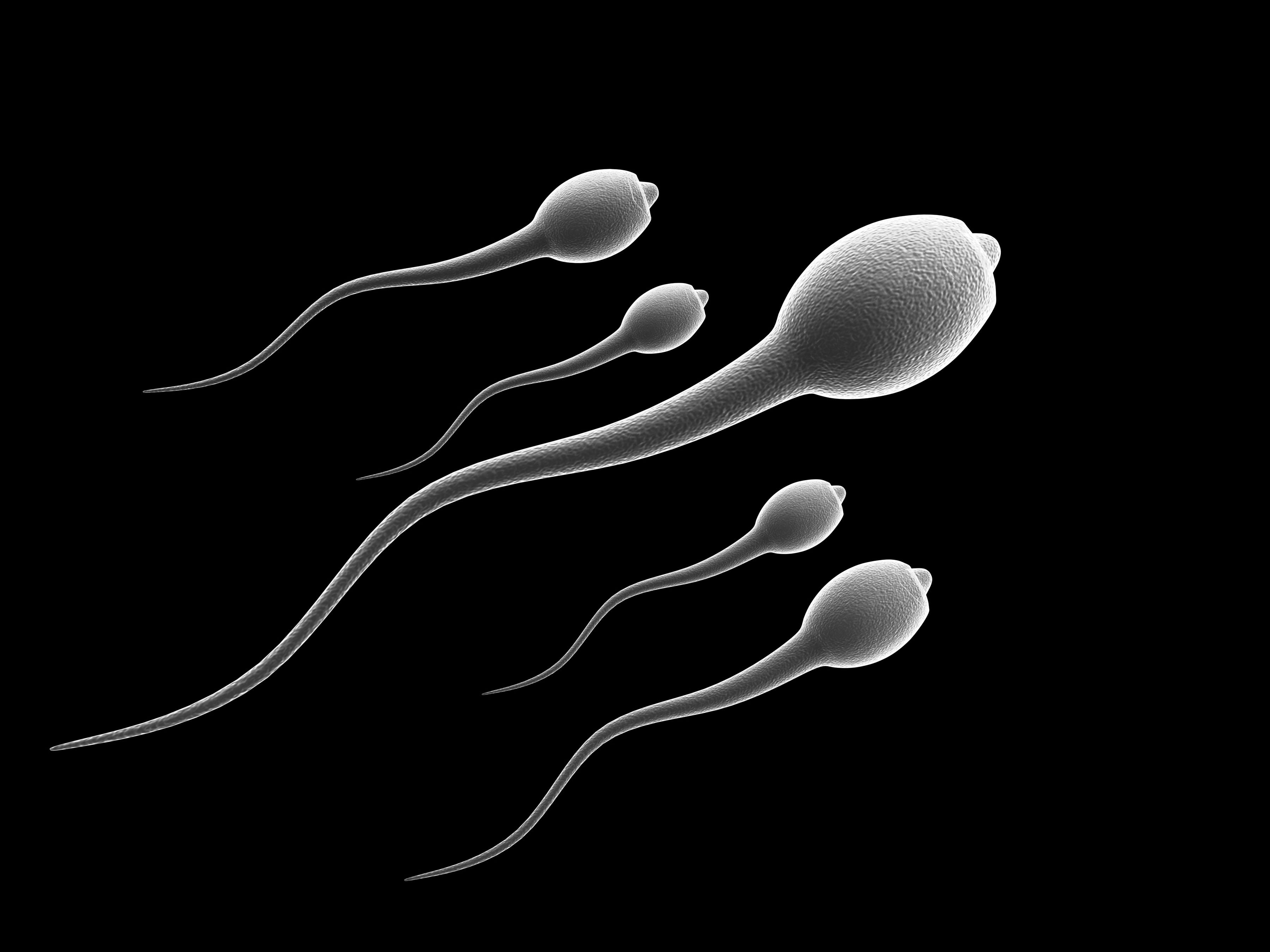
Sperm are not visible to the human eye, however when viewed under a microscope they look a bit like tadpoles because they have a round head section and a long tail. The head of a sperm contains it nucleus , within which 23 chromosomes (i.e. tiny rod like structures which contain genetic information called DNA) are housed. The tail structure enables the sperm to move actively once it leaves the testicles. It helps propel sperm forward from the vagina (when sperm are expelled during sexual intercourse) toward the uterus in search of an oocyte in the fallopian tubes. The tail also provides the necessary motion for the sperm to bind to and penetrate an egg once it has been reached.
In order to fertilise an egg and create an embryo, sperm must leave the testes and come into contact with a mature oocyte (i.e. an oocyte which is ready for fertilisation). Oocytes mature within ovarian follicles in a woman’s ovaries. Typically a single ovarian follicle will prepare an oocyte for release during each ovulatory cycle , and thus, a single mature oocyte will be released each time a woman ovulates. The oocyte is released from the follicle where it has matured, then leaves the ovaries and travels to the uterus via the fallopian tubes , usually every 28 days. For fertilisation to occur, sperm must enter the fallopian tubes while the mature oocyte is also there (i.e. just after the oocyte has been released from its follicle).
Sperm typically enter the fallopian tubes following unprotected sexual intercourse, during which a man’s testicles are stimulated to release sperm upon orgasm. Sperm leaves the testicles, via the epididymis and vas deferens (i.e. the tubes linking the testes to the urethra ), where they combine with other fluids, known as the seminal fluids . The seminal fluid leaves the body via the urethral opening of the penis. If ejaculation occurs during unprotected sexual intercourse (i.e. while the man’s penis in inserted in the woman’s vagina without a protective barrier) the sperm will enter the vaginal cavity. If the sperm are motile (i.e. have the ability to move around or ‘swim’) they will travel up the vaginal tract to the cervical opening. Sperm must then travel through a layer of mucus which protects the cervical opening, before entering the woman’s uterus and fallopian tubes, where they may reach an egg.
In many cases the woman will not be ovulating at the time of sexual intercourse, therefore no mature oocyte will be present in the fallopian tubes and fertilisation will not occur. If there is a mature oocyte in the woman’s fallopian tubes and sperm are healthy, sperm will be attracted to the oocyte and attempt to swim to it, bind to its surface and eventually penetrate its zona pellucida (i.e. shell). Once the sperm has penetrated the zona pellucida it enters the nucleus of the egg, where the egg’s chromosomes (which contain the maternal DNA) are stored. When the sperm head penetrates the zona pellucida the 23 chromosomes contained in the sperm head join with the 23 chromosomes in the egg’s nucleus and form an embryo with 46 chromosomes (i.e. the number of chromosomes found in all normal human cells except gametes). The single celled embryo will then replicate to produce further 46 chromosome cells which will eventually form the foetus. It is this process of the egg and sperm combining their chromosomes which represents the end of the fertilisation process.
Male factor infertility occurs when problems resulting from the man’s sperm prevent a couple from conceiving. It affects about one in twenty Australian men and is most commonly underpinned by sub-optimal sperm production . Sub-optimal sperm production is a condition in which a man fails to produce a sufficient quantity of sperm or produces sperm of a low quality (e.g. abnormally shaped sperm).
When a man produces a low number of sperm, the concentration of sperm in the ejaculate is much lower than in a man with healthy sperm production. Thus, the chance that one of the millions of sperm contained in the seminal fluid which is ejaculated upon orgasm will reach an oocyte in the woman’s fallopian tubes is greatly reduced.
The production of low quality sperm also reduces the chance of fertilisation. Low quality sperm are typically either immotile (i.e. they cannot move) or abnormally shaped, or both. Sperm which are immotile cannot travel up the vaginal tract and into the uterus, and thus cannot locate and fertilise a mature oocyte. Those which are abnormally shaped may or may not be able to move, however even if they manage to travel to an oocyte, they will usually be unable to bind to and penetrate its shell and the couple will be unable to conceive as a result.
In a minority of cases of male factor infertility, sperm production occurs normally in the testicles, but difficulties arise in the process of ejaculating sperm. Some men completely fail to ejaculate and this may result from spinal cord injuries, injuries to the testicles, or testicular conditions such as infection or cryptorchidism . Other men will be able to ejaculate, however their seminal fluid will not contain sperm. These cases are most commonly caused by obstructions in the epididymis and vas deferens (e.g. due to infection). In other cases of male factor infertility, ejaculation occurs however the sperm do not enter the woman’s vagina. For example retrograde ejaculation is a condition in which a man ejaculates into his bladder, and thus ejaculate is not expelled into a woman’s vagina, even if ejaculation occurs during sexual intercourse.
Male factor infertility can be diagnosed by a sperm analysis (sperm count test) .
Sperm retrieval is the process of retrieving sperm from a man for semen analysis testing or for use in assisted reproductive techniques .
Regardless of the intended use, sperm is of optimal quality when it is fresh, so whenever possible should be retrieved around an hour before it will be used. The sample should be collected after not less than 48 hours and not more than 7 days of sexual abstinence.
In cases where it is not practical or possible to retrieve sperm on the day of its intended us, sperm may be retrieved in advance, however it must then be cryopreserved and thawed immediately before use.
There are a number of ways in which sperm can be retrieved, and the technique used will depend upon the factors causing the man’s fertility. The easiest and most common method is through ejaculation, however for men who are unable to ejaculate their sperm, or those who ejaculate only immotile sperm, there are also surgical and electro-stimulation techniques which are often successful in retrieving sperm. The collection of sperm from morning urine is also possible and while this technique has not yet been applied to infertility treatment, it is used to successfully retrieve sperm for other clinical purposes.
Ejaculation is the natural process through which a man’s body expels sperm and it occurs as a result of sexual stimulation, coinciding with the man’s orgasm. Masturbation is the technique most commonly used to induce ejaculation for sperm retrieval purposes. It is a relatively simple technique, which the patient can perform without the assistance of a health professional.
Masturbation provides a complete semen sample, which is important for both semen analysis testing and assisted reproduction, because the first quantity of seminal fluid expelled during ejaculation is typically of the best quality.
Results will therefore be inaccurate or outcomes less than optimal, if this portion of the ejaculate is not captured. Masturbation is also the preferred technique for sperm retrieval because it provides a semen sample that is uncontaminated (e.g. by vaginal fluids).
So that a man can induce ejaculation through masturbation in comfort and privacy, most infertility clinics provide a private room in which the man, and if necessary his partner, can perform masturbation. The man will be provided with a sterile container, labelled with identifying information, in which the ejaculate can be stored. He will be instructed to check the identifying information to ensure it is his, then to ejaculate into the container and ensure all the ejaculate, and particularly the first portion, is captured. The semen specimen should then be handed immediately to the treating clinicians, who will record the date and time of ejaculation and store the semen sample at room temperature if it is to be used immediately, or cryopreserve it for future use.
For men who find it difficult to achieve orgasm and ejaculate in the clinic environment, some clinics allow the male partner to complete sperm retrieval at home. There are no significant differences in pregnancy rates following intrauterine insemination when sperm is retrieved at home or in a clinic, as long as the sperm sample reaches the clinic quickly (i.e. one hour). When sperm retrieval is performed at home, the man will be provided with a sterile container, labelled with the couple’s identifying information, in which to collect his ejaculate. The time and date of collection should be recorded on the jar, immediately following ejaculation. The patient will be instructed to seal the container and ensure it is kept at room temperature until it reaches the clinic. Because sperm performs better when it is fresh, it is important that the sample reaches the clinic within one hour of ejaculation. For patients who are geographically remote from infertility clinics or do not have reliable forms of transport to reach the clinic, home retrieval is therefore not an option.
Inducing ejaculation by engaging in sexual intercourse is generally not recommended for sperm retrieval purposes. However if the man’s personal or religious beliefs exclude the use of masturbation, clinics may permit the use of intercourse to induce ejaculation. In such cases, couples will be provided with a special condom to use to collect the semen sample. Couples will be advised not to use a standard condom as normal latex condoms affect the quality of the semen sample. Couples will also be advised against coitus interuptus (i.e. the technique in which intercourse is interrupted and the penis withdrawn from the vagina immediately prior to ejaculation). This is because the best quality portion of the semen is ejaculated first and may not be captured using this technique, but also because vaginal fluid can affect the quality of the semen sample.
For men who do not produce ejaculate, vibration or electro stimulation techniques are often effective in inducing ejaculation. They are relatively simple techniques which do not require anaesthetic, however they do require the assistance of a health professional and special medical equipment. The vibro-stimulation technique involves holding a special vibrating instrument to a man’s penis. The aim is to induce an ejaculation by stimulating ejaculatory reflexes. The electro stimulation technique involves inserting a electro-stimulation probe into the man’s rectum. Electrical impulses are then sent through the probe to stimulate sensitive nerves in this region, which can induce an erection and ejaculation.
When other sperm retrieval techniques fail, there are several surgical methods which can be used to retrieve sperm from either the epididymis or testicles. They are:
There is currently insufficient evidence to determine which of the sperm retrieval techniques have the best outcomes in terms of pregnancy rates or patient satisfaction.
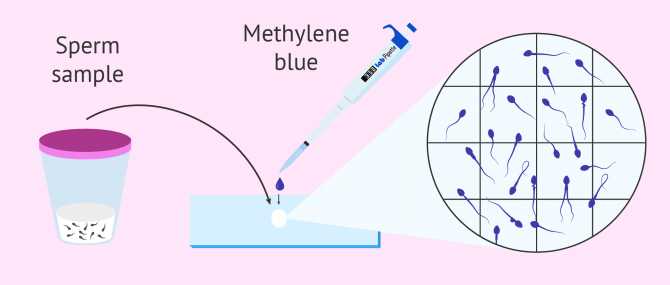
Semen analysis testing, also known as a sperm count test, is the main test which is performed to assess a man’s fertility. It involves examining a sample of freshly retrieved semen under a microscope and by conducting a range of tests. Semen analysis is most commonly performed manually, however computer assisted semen analysis can increase the accuracy of the assessment if specialised equipment is available. Microscopic investigation involves a highly trained professional placing a small amount of sperm onto a slide and examining it under a microscope.
The results are compared to reference values published by the World Health Organisation. Semen analysis testing investigates a number of characteristics of the seminal fluid and the sperm it contains including:
The results of a semen analysis test will be compared to reference values determined by the World Health Organisation (WHO) . When conducting semen analysis testing it is important to remember that assessment of the entire population of sperm in a sample of ejaculate does not determine whether or not a man has the capacity to conceive naturally (i.e. through sexual intercourse). A man with low sperm concentration still has the capacity to conceive naturally, although his likelihood of conception will be reduced compared to a man with a higher concentration of sperm.
Analysis of the total quality and quantity of sperm in an infertile man is conducted as it allows clinicians to gain insight regarding the factors which are likely underpinning the couple’s infertility problems, but not because it enables clinicians to predict the likelihood of natural conception occurring at some point in the future.
When the results of the semen analysis fall within the parameters outlined by WHO (, the man’s sperm production is considered normal. When one or more of the test values fall outside the WHO criteria, a repeat semen analysis test is usually conducted (ideally 3 months after the first test) to confirm the result. Semen quality can vary considerably over time, due to the health, lifestyle and environmental conditions of the man whose semen is being analysed. Around 10% of men who return abnormal results in their first semen analysis test will actually have normal results when they are tested again.
World Health Organisation Reference Values for Semen Analysis Testing 3
Based on the results of semen analysis testing, a man will be given a sperm classification, using the following standard terminology:
The type of infertility treatment which will be most effective in achieving conception varies depending on the characteristics of each patient’s semen.
Following retrieval, sperm will be taken to a laboratory for analysis or preparation for assisted reproductive techniques. As a semen sample potentially contains dangerous viruses (e.g. hepatitis virus) clinicians must handle it as a hazardous substance (e.g. ensure it does not come into contact with their skin). When sperm is used for assisted reproductive procedures, it is also important that the sperm be prepared using sanitary techniques to prevent the introduction of bacteria into the female patient’s uterus.
Sperm preparation is a procedure in which the most viable sperm in an ejaculate (i.e. the most morphologically normal and motile) are separated from non-viable and dead sperm, white blood cells and bacteria in the suspension. This is because these components of the suspension are thought to impair the fertilisation process. Following separation, the motile sperm are re-suspended to form a solution with a high concentration of sperm.
There are a range of techniques which can be used to prepare sperm and the technique used will depend upon the assisted reproductive technique procedure and the quality of the semen sample. The procedures use different techniques, however are similar in that they all aim to separate viable from non-viable sperm.
The most common semen preparation techniques are:
Find practitioners near you and book your next appointment online.
> 50% progressive or
> 25% rapidly progressive
Immunobead or mixed antiglobulin reaction test*
For more information on sperm health and male fertility, see Sperm Health .
For more information on infertility, including investigations and treatments, as well as some useful animations, see Infertility .
Sensual Jane 18
Lingerie Photo Galleries
Www Peeing Video
Girls Breast Naked
Nipple Penetration

























/arc-anglerfish-arc2-prod-dmn.s3.amazonaws.com/public/QMNKT4TUW5GNAABJOQGPDKIZWQ.jpg)