Rectal Prolapse
⚡ ALL INFORMATION CLICK HERE 👈🏻👈🏻👈🏻
Rectal Prolapse
Medically reviewed by Michele Cho-Dorado, M.D. — Written by Tom Seymour on November 11, 2017
A rectal prolapse tends to become noticeable gradually over time. Often it is associated with weak muscles in the pelvis. There can be complications if it is not treated promptly and properly. Treatment will depend on age, general health, and the cause of the prolapse.
Share on Pinterest Rectal prolapse may be internal or external.
Share on Pinterest A prolapsed rectum may cause a number of symptoms, inluding constipation and bleeding from the rectum.
Share on Pinterest If constipation cannot be treated, surgery may be recommended for treating the rectal prolapse.
Medically reviewed by Michele Cho-Dorado, M.D. — Written by Tom Seymour on November 11, 2017
Medically reviewed by University of Illinois
© 2004-2021 Healthline Media UK Ltd, Brighton, UK, a Red Ventures Company. All rights reserved. MNT is the registered trade mark of Healthline Media. Any medical information published on this website is not intended as a substitute for informed medical advice and you should not take any action before consulting with a healthcare professional
© 2004-2021 Healthline Media UK Ltd, Brighton, UK, a Red Ventures Company. All rights reserved. MNT is the registered trade mark of Healthline Media. Any medical information published on this website is not intended as a substitute for informed medical advice and you should not take any action before consulting with a healthcare professional
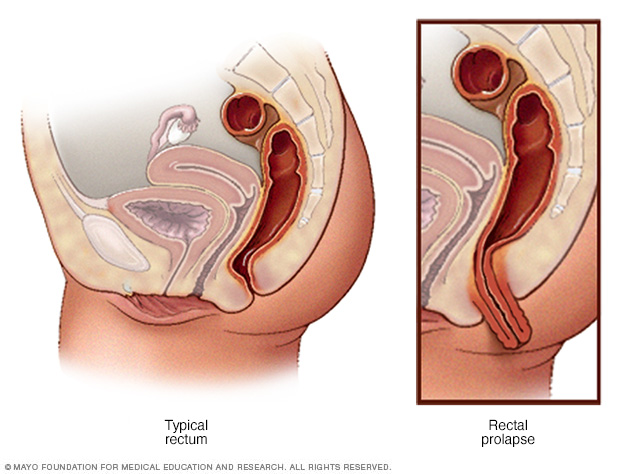
Rectal prolapse is when part of the rectum protrudes from the anus. The rectum is the last part of the large intestine and is where feces is stored before being passed.
Prolapse occurs when the rectum becomes unattached inside the body and comes out through the anus, effectively turning itself inside out.
Rectal prolapse is a relatively rare condition, with the American Society of Colon and Rectal Surgeons estimating that it affects less than 3 in every 100,000 people .
There are three types of rectal prolapse:
There is a range of risk factors and causes associated with rectal prolapse, although doctors do not fully understand why some people get it.
It can be triggered by a variety of things including:
There are also some neurological conditions that affect the nerves associated with rectal prolapse:
Rectal prolapse is more common in adults than children, and it is particularly prevalent in women aged 50 years or older, who are six times more likely to be affected than men.
Most women who have rectal prolapse are in their 60s, while most men are aged 40 or younger.
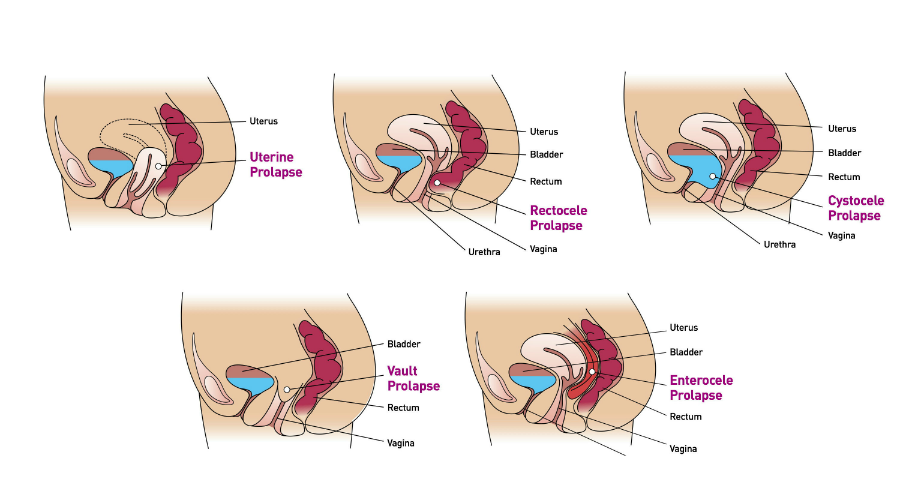
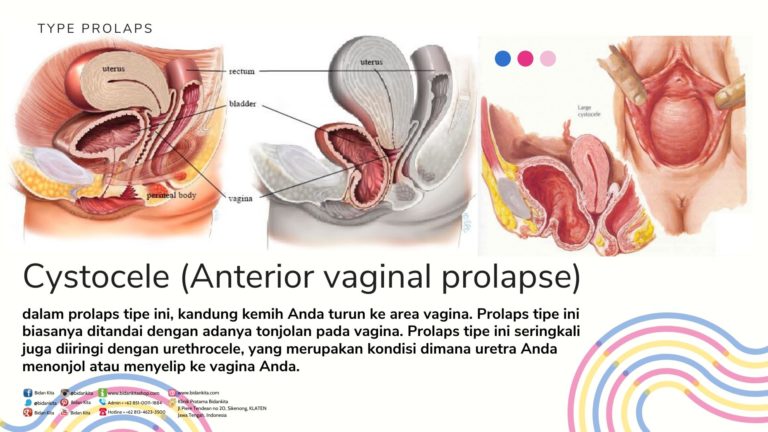
In the case of older women, rectal prolapse will often occur at the same time as a prolapsed uterus or bladder. This is because of general weakness in the pelvic floor muscles.
At first, the person might only notice a lump or swelling coming out of their anus when they have a bowel movement.
Initially, the person may be able to push the rectal prolapse back in. Over time, however, the prolapse is likely to protrude permanently, and a person will be unable to push the prolapse back.
As time goes on, a rectal prolapse may happen when a person coughs, sneezes, or stands up. Some people with a rectal prolapse have described it as like “sitting on a ball.”
Some people may experience an internal rectal prolapse, which is different in that the prolapse will not protrude. However, the person may feel as if they have not passed everything during a bowel movement.
Other symptoms of a rectal prolapse include:
Although a rectal prolapse is not often defined as an emergency medical problem, it can be uncomfortable, embarrassing, and have a significant adverse effect on the person’s mental and physical life.
Therefore it is essential for anyone who has noticed any signs or symptoms of rectal prolapse to see a doctor as soon as possible.
The longer a person puts off receiving treatment for rectal prolapse the greater chance of permanent problems, such as incontinence and nerve damage.
In order to diagnose a rectal prolapse, the doctor will look at the person’s medical history, ask them about their symptoms, and conduct a physical examination.
A physical examination will involve the doctor inserting a lubricated, gloved finger into the rectum. While this can be uncomfortable and possibly embarrassing, it should not be painful and is very important for an accurate diagnosis.
Further tests may be required to clarify the diagnosis or rule out other processes, which include:
In the first instance, it is important to treat constipation. This might be achieved by eating plenty of foods that are high in fiber, such as fruit, vegetables, and wholegrains.
Bulking laxatives, which help a person have a bowel movement without straining, may also be recommended, as well as drinking plenty of water.
If that does not work, then surgery may be advised. The type of surgery will depend on a number of factors:
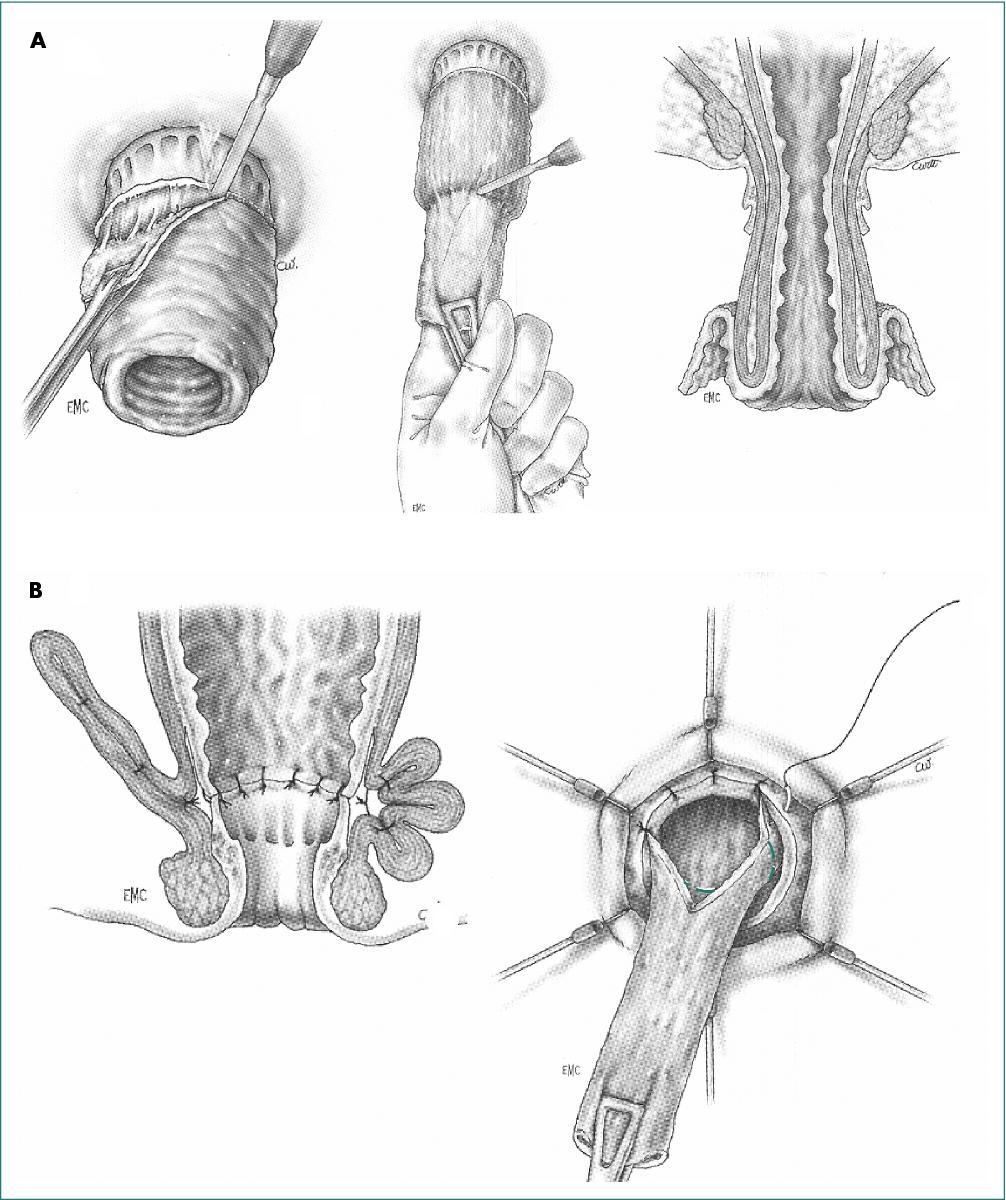
There are two general types of surgery for rectal prolapse:
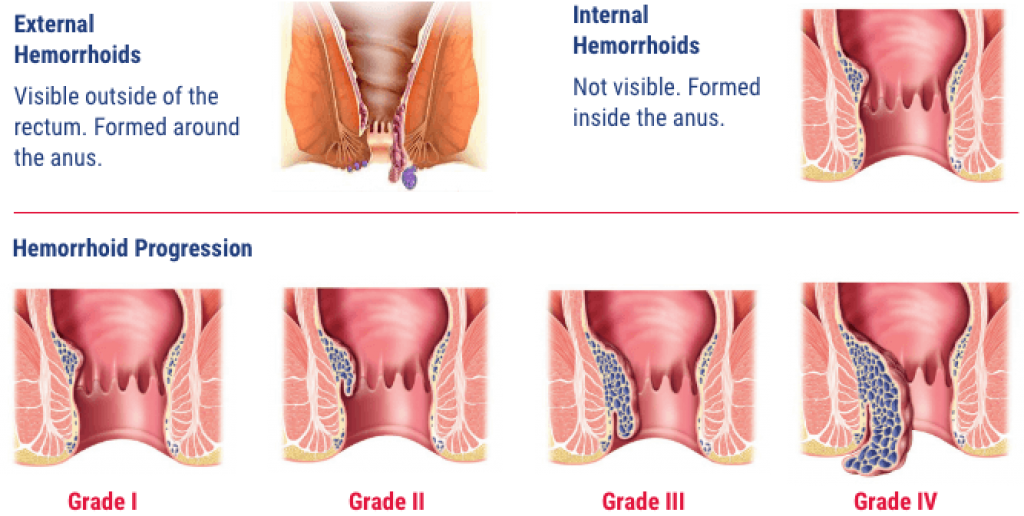
Rectal prolapse can be confused with hemorrhoids , which are also known as piles . This is because both conditions affect the last section of the bowel and have similar symptoms.
While rectal prolapse affects the rectal wall, hemorrhoids affect the blood vessels in the anal canal. These two conditions require different treatment, so it is important to get the correct diagnosis.
There are some lifestyle changes people can make to try and avoid rectal prolapse, including :
Most people make a full recovery after treatment for rectal prolapse and lead a normal life.
However, proper recovery is crucial and how long this will take will depend on the type of treatment.
Typically, people who have had surgery spend 3 to 5 days in the hospital after the operation, and most make a complete recovery within 3 months. After undergoing surgery for a rectal prolapse, people should avoid straining and heavy lifting for at least 6 months afterward.
Last medically reviewed on November 11, 2017
Rectal Prolapse : Symptoms, Causes, Treatment, Surgery
Rectal prolapse : Causes, symptoms, and treatments
Rectal Prolapse Symptoms, Surgery, Treatment, Causes & Recovery
Rectal Prolapse | Cedars-Sinai
Rectal Prolapse . Symptoms of rectal prolapse and treatment. | Patient
This website uses cookies to deliver its services as described in our Cookie Policy . By using this website, you agree to the use of cookies.
Medical Author:
John P. Cunha, DO, FACOEP
Medical Editor:
BS Anand, MD
What Facts Should I Know About Rectal Prolapse?
Do Hemorrhoids Cause Rectal Prolapse?
What Are the Symptoms of Rectal Prolapse?
Can Medication Cure Rectal Prolapse?
What Home Remedies Treat and Relieve Pain?
How Can You Prevent Rectal Prolapse?
What Is the Prognosis for Rectal Prolapse? Can It Recurr?
What Does Rectal Prolapse Look Like (Pictures)?
Health Solutions From Our Sponsors
Shot-Free MS Treatment
Your Child and COVID-19
Rodriguez, LA, et al. "Rectal prolapse in children." UpToDate. Dec. 2018. .
Varma, Madhulika GM, et al. "Overview of rectal procidentia (rectal prolapse)." UptoDate. Dec. 2018. .
CONTINUE SCROLLING FOR RELATED SLIDESHOW
You are about to visit a website outside of emedicinehealth . Please familiarize yourself with this other website's Privacy Policy as it differs from ours.
You are about to visit a website outside of emedicinehealth . Please familiarize yourself with this other website's Privacy Policy as it differs from ours.
First Aid & Emergencies
Topics A-Z
Slideshows
Images
Quizzes
Medications
About Us
Privacy
Terms of Use
Advertising Policy
Site Map
Contact Us
Do Not Sell My Personal Information
WebMD
Medscape Reference
Medscape
MedicineNet
RxList
OnHealth
WebMDRx
©2021 WebMD, Inc. All rights reserved.
eMedicineHealth does not provide medical advice, diagnosis or treatment.
See Additional Information.
WebMD processes personal data about users of our site, including health data, through the use of cookies to deliver our services, personalize advertising and to analyze site activity. We may share certain information about our users with our advertising and analytics partners. For additional details, refer to the WebMD Privacy Policy and WebMD Cookie Policy .
By clicking "I AGREE" below, you agree to the WebMD Privacy Policy and WebMD Cookie Policy and WebMD’s personal data processing and cookie practices as described therein.
©2018 WebMD, Inc. All rights reserved. eMedicineHealth does not provide medical advice, diagnosis or treatment. See Additional Information.
©1996-2021 WebMD , Inc. All rights reserved. Terms of Use.
eMedicineHealth does not provide medical advice, diagnosis or treatment. See additional information .
The rectum refers to the lowest 12-15 centimeters of the large intestine . The rectum is located just above the anal canal. Normally, the rectum is securely attached to the pelvis with the help of ligaments and muscles that hold it in place.
Causes of rectal prolapse include factors such as age of 40 years, long-term constipation , the stress of childbirth, or large hemorrhoids (large, swollen veins inside the rectum) that may cause these ligaments and muscles to weaken, causing the rectum to prolapse, meaning it slips or falls out of place. Other risk factors of include long-term diarrhea , long-term straining during defecation, previous surgery, cystic fibrosis, chronic obstructive pulmonary disease , whooping cough , multiple sclerosis , and paralysis.
Signs and symptoms of include pain during bowel movements, mucus or blood discharge from the protruding tissue, fecal incontinence , a loss of urge to defecate, and awareness of something protruding upon wiping.
Medical treatment helps ease the symptoms of a prolapsed rectum temporarily or to prepare the patient for surgery. Bulking agents, stool softeners, and suppositories or enemas are used as treatment to reduce pain and straining during bowel movements.
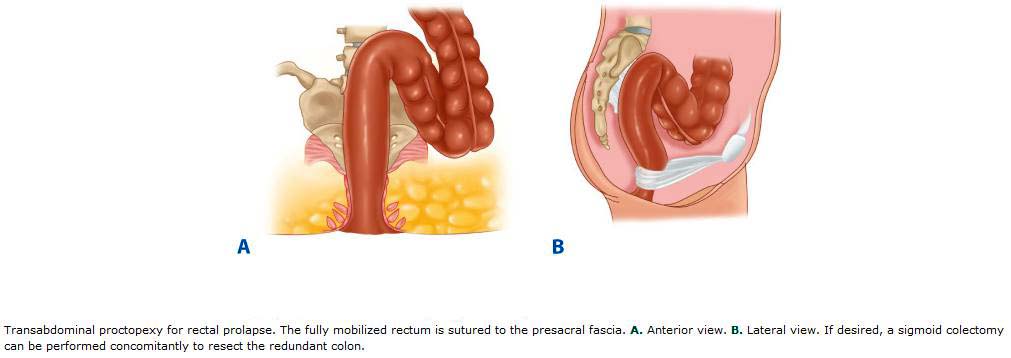
Surgery to repair of this condition usually is performed by a colorectal surgeon and involves attaching or securing the rectum to the back side (or posterior) part of the inner pelvis.
The outlook for a patient with this health condition generally is good, and most people recover well after surgery.
Prevention of involves eating a high-fiber diet and drinking plenty of fluids to reduce constipation ; avoid straining during bowel movements; treat any long-term diarrhea , constipation, or hemorrhoids .
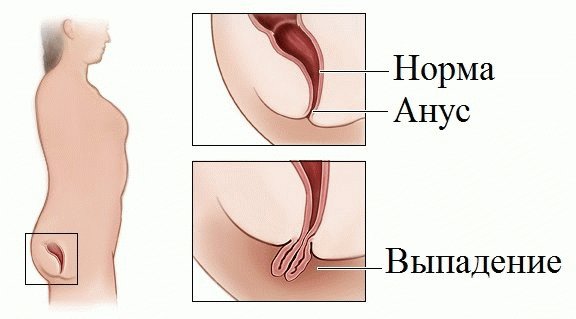
The term rectum refers to the lowest 12-15 centimeters of the large intestine ( colon ). The rectum is located just above the anal canal (the junction is called the anorectal area). Normally, the rectum is securely attached to the pelvis with the help of ligaments and muscles that hold it in place. When these ligaments and muscles weaken, the rectum can slip or fall out of place, or prolapse (also called rectal procidentia).
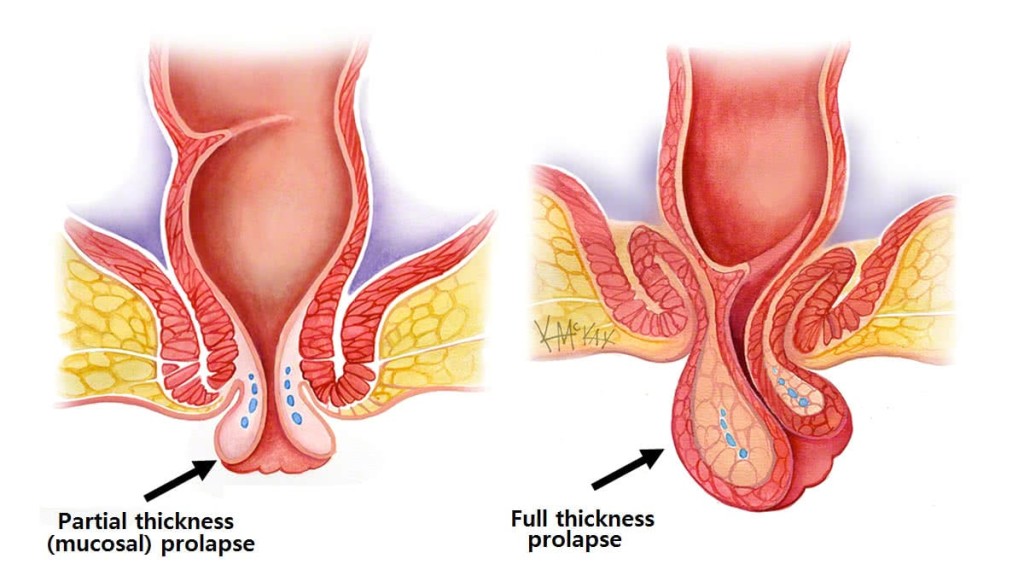
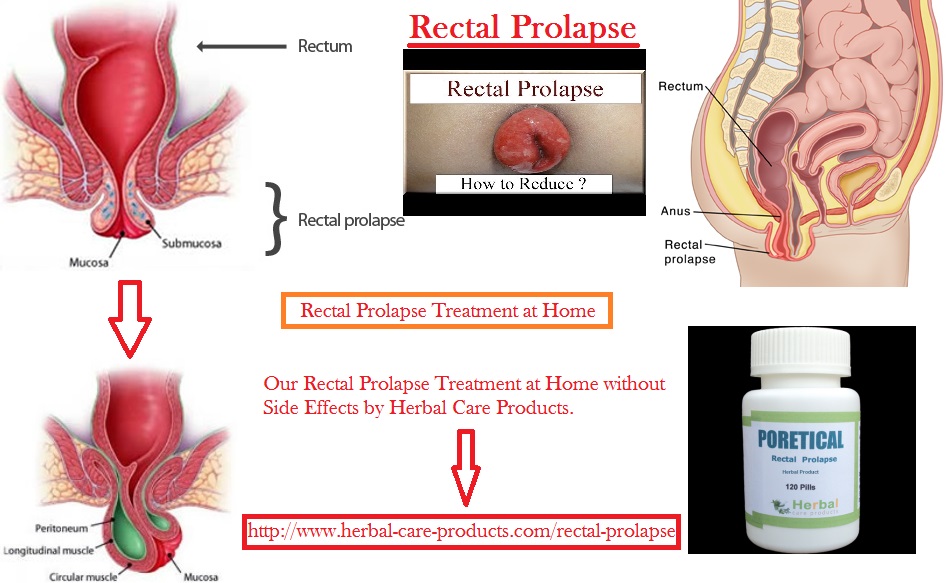
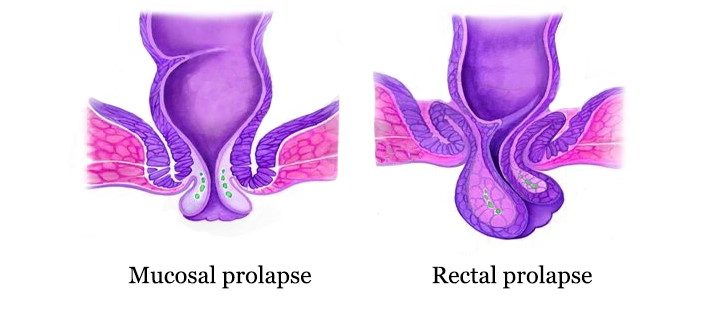
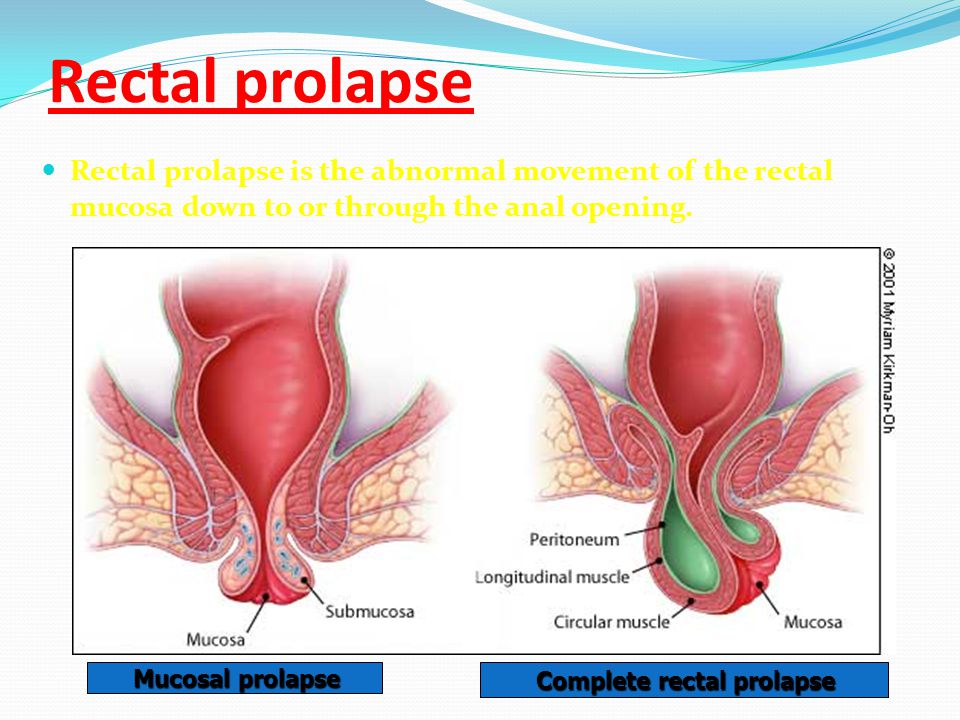
In the early stages of rectal prolapse, the rectum becomes poorly attached but stays within the body most of the time. This stage is called mucosal prolapse, or partial prolapse, meaning that only the inner lining of the rectum (rectal mucosa) protrudes from the anus. This occurs when the connective tissues within the rectal mucosa loosen and stretch, allowing the tissue to protrude through the anus. When long-term hemorrhoidal disease is the cause, the condition usually does not progress to complete prolapse. Determining if the problem is hemorrhoids or rectal prolapse is important. Hemorrhoids occur commonly, but they rarely cause the condition.
As the rectum becomes more prolapsed, the ligaments and muscles may weaken to the point that a large portion of the rectum protrudes from the body through the anus. This stage is called complete prolapse, or full-thickness rectal prolapse, and is the most commonly recognized stage of the condition. Initially, the rectum may protrude and retract depending on the person's movements and activities. However, if the disease goes untreated, the rectum may protrude more frequently or even permanently.
Rectal prolapse is similar to, but not the same as, a rectocele, a common condition in women, where the rectum falls forward into the backside (or posterior) wall of the vagina, causing a lump inside the vagina.
Another condition commonly considered a form of prolapsed rectum is called internal intussusception. Its effects on the rectum are similar to those of mucosal prolapse or complete rectal prolapse; however, in internal intussusception, the rectum neither protrudes from the body nor enters the anal canal.
Rectal prolapse is caused by weakening of the ligaments and muscles that hold the rectum in place. In most people with a prolapsed rectum, the anal sphincter muscle is weak. The exact cause of this weakening is unknown; however, risk factors usually are associated with the following health conditions.
Long-term hemorrhoidal disease is frequently associated with mucosal prolapse (partial prolapse) that does not progress to complete prolapse of the rectum.
The symptoms of a prolapsed rectum are similar to those of hemorrhoids; however, it originates higher in the body than hemorrhoids do. A patient with the condition may feel tissue protruding from the anus and experience the following symptoms:
Early in the development of this condition, the protrusion may occur during bowel movements and retract afterwards. The protrusion may become more frequent and appear when the patient sneezes or coughs . Eventually, the protruding rectum may need to be manually replaced or may continually protrude.
Patients with internal intussusception in which the rectum is displaced but does not protrude from the body, often experience difficulty with bowel movements and a sense of incomplete bowel movements.
To confirm the presence of a prolapsed rectum, the doctor may ask the person to sit on the toilet and strain. If the rectum does not protrude, the doctor may administer a phosphate enema to confirm the diagnosis. The main condition to distinguish prolapse of the rectum from is protruding or prolapsing hemorrhoids.
A defecogram (a test that evaluates bowel control) may help distinguish between a mucosal prolapse and a complete prolapse of the rectum in a patient.
Almost all cases require medical care, and in most cases, surgery is required to treat and cure the problem. Most cases will worsen without surgery. Occasionally, successful treatment of an underlying cause of a prolapsed rectum may resolve the problem. However, these scenarios usually involve infants or children. The cause of this condition in many patients are constipation or straining while having a bowel movement. These tips may help ease bowel movements and ease symptoms.
The treatment standard to cure rectal prolapse is surgery. Medical treatment is normally used to ease the symptoms of a prolapsed rectum temporarily or to prepare the patient for surgery. Bulking agents (such as bran or psyllium), stool softeners, and suppositories or enemas are used for these purposes.
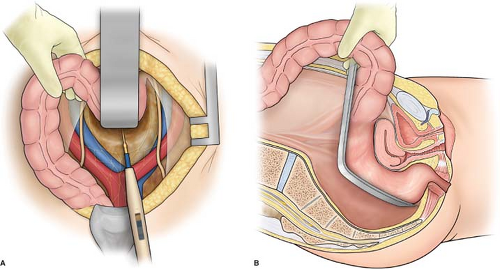
Surgery through the abdomen typically performed in younger or healthier patients. The type of abdominal surgery usually determined by severity of associated constipation. Associated with higher morbidity rate than perineal approach but lower recurrence rate of prolapse performed under general anesthesia.
The perianal approach is typically performed in elderly people or people in poor health who cannot tolerate general anesthesia. The perianal approach is associated with higher recurrence rate than abdominal approach, and usually involves a shorter hospital stay.
If a patient is too weak for surgery, a doctor can prevent a prolapse by inserting a wire or plastic loop to hold the sphincter closed.
After surgery, a Foley catheter may be left in place for a day or two and the patient may need to follow a liquid diet until normal bowel functions return.
A perineal surgery may require one to three days in the hospital, and abdominal surgery may require up to a week.
The recovery time following either type of surgery is several weeks and involves adding fiber to the diet and avoiding:
The patient will likely need one or two follow-up visits to their doctor within the first month after surgery to check that incisions are healing well and to make sure bowel movements are normal.
With timely and appropriate treatment, most people who undergo surgery experience few or no symptoms related to rectal prolapse after surgery. Several factors, including age, severity of the prolapse, type of surgical approach, and health of the patient, contribute to the quality and speed of a person's recovery.
Rectal pain has many causes. Common causes are hemorrhoids, anal fissures, and fleeting spasms. Less common causes of may include:
































 f_auto" width="550" alt="Rectal Prolapse" title="Rectal Prolapse">w_1920/v1560143800/gu0t0urovobjh05qzvgo.jpg" width="550" alt="Rectal Prolapse" title="Rectal Prolapse">
f_auto" width="550" alt="Rectal Prolapse" title="Rectal Prolapse">w_1920/v1560143800/gu0t0urovobjh05qzvgo.jpg" width="550" alt="Rectal Prolapse" title="Rectal Prolapse">