Prolapsed Man
🛑 👉🏻👉🏻👉🏻 INFORMATION AVAILABLE CLICK HERE👈🏻👈🏻👈🏻
https://academic.oup.com/gastro/article/7/4/279/5487275
Introduction
Methods
Results
Discussion
Authors’ Contributions
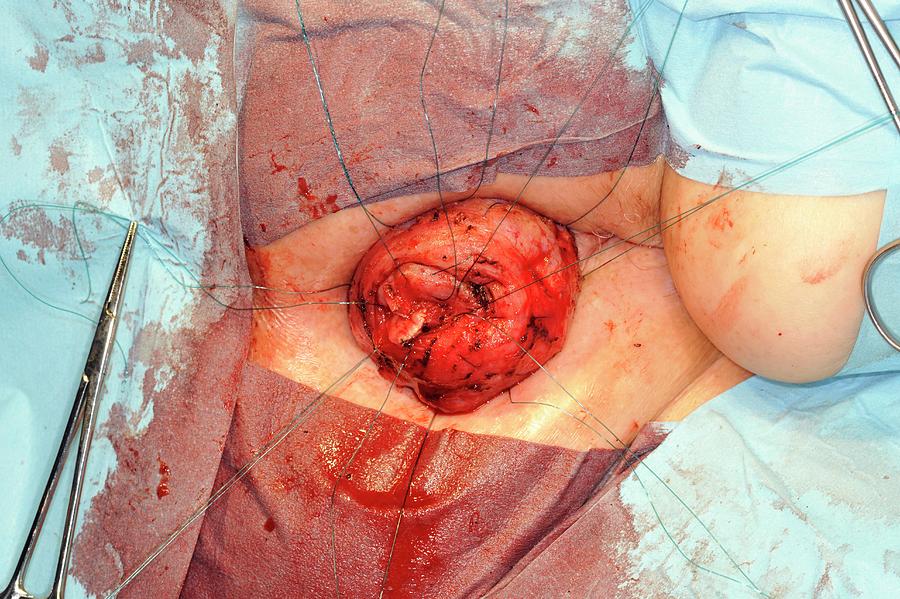
Full-thickness rectal prolapse is a benign, but stressful, condition that leads to problems with bleeding, fecal incontinence and obstructed defecation [1–8]. Rectal prolapse can significantly affect quality of life and therefore should be repaired whenever possible. Older women are the most commonly affected group. Multiple risks fact…
https://m.youtube.com/watch?v=CQAxALbTMR4
Great Reactions of the 21st Century - Prolapse Man
Man’s Rectum FALLS OUT While Playing Phone Games
Rectal prolapse ( complete full thickness ) being reduced - Dr Narotam Dewan
YouTube › Dr Narotam-Dewan-Hospital Ludhiana
Altemeier proctectomy procedure illustrated Gopro High Definition
How Old is Too Old for Pelvic Organ Prolapse Surgery?
Man stomps on woman's head before driving into service station
https://en.m.wikipedia.org/wiki/Rectal_prolapse
Specialty: General surgery
Other names: Complete rectal prolapse, external rectal prolapse
Rectal prolapse is when the rectal walls have prolapsed to a degree where they protrude out the anus and are visible outside the body. However, most researchers agree that there are 3 to 5 different types of rectal prolapse, depending on if the prolapsed section is visible externally, and if the full or only partial thickness of the rectal wall is involved.
Rectal prolapse may occur without any symp…
Rectal prolapse is when the rectal walls have prolapsed to a degree where they protrude out the anus and are visible outside the body. However, most researchers agree that there are 3 to 5 different types of rectal prolapse, depending on if the prolapsed section is visible externally, and if the full or only partial thickness of the rectal wall is involved.
Rectal prolapse may occur without any symptoms, but depending upon the nature of the prolapse there may be mucous discharge (mucus coming from the anus), rectal bleeding, degrees of fecal incontinence and obstructed defecation symptoms.
Rectal prolapse is generally more common in elderly women, although it may occur at any age and in either sex. It is very rarely life-threatening, but the symptoms can be debilitating if left untreated. Most external prolapse cases can be treated successfully, often with a surgical procedure. Internal prolapses are traditionally harder to treat and surgery may not be suitable for many patients.
Solitary rectal ulcer syndrome and colitis cystica profunda
https://www.guysandstthomas.nhs.uk/resources/patient-information/gynaecology/treating...
Members of Guy’s and St Thomas’ NHS Foundation Trust contribute to the organisation on a voluntary …
https://www.verywellhealth.com/what-is-rectal-prolapse-1945061
Who Is Likely to Experience A Rectal Prolapse?
Symptoms
Causes
Treatment
Although rectal prolapse can affect anyone, it is most common in adults, and women ages 50 and older have six times the risk as men.1 It occurs in children, usually between infancy and 4 years of age, who have an un…
Rectal prolapse in men is a rare condition and overall comprises only a small proportion of rectal-prolapse cases [ 9–11 ]. The focus of this study was to examine rectal prolapse in the male population and evaluate surgical options for the repair of rectal prolapse in this population.
academic.oup.com/gastro/article/7/4/279/…
Rectal prolapse occurs when the rectum becomes stretched out and protrudes from the anus. Rectal prolapse occurs when part of the large intestine's lowest section (rectum) slips outside the muscular opening at the end of the digestive tract (anus). The prolapsed rectum can cause fecal incontinence.
www.mayoclinic.org/diseases-conditions/r…
What is the best surgery for prolapse?
What is the best surgery for prolapse?
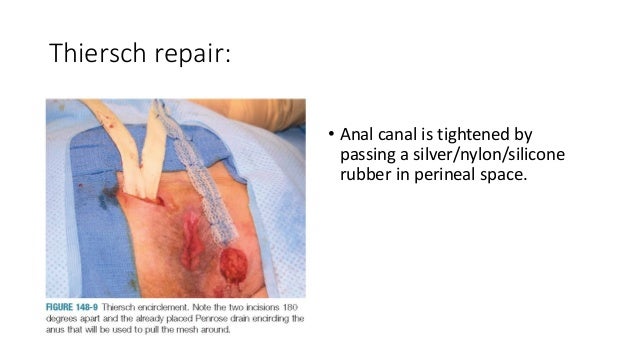
There are a number of different operations to correct a prolapse, but the main aim of surgery is to lift the organ(s) back into place. Your consultant will discuss the surgical options with you and recommend which is best for you after taking your age, type of prolapse and general health into consideration.
www.guysandstthomas.nhs.uk/resources/p…
What does prolapse of the womb mean?
What does prolapse of the womb mean?
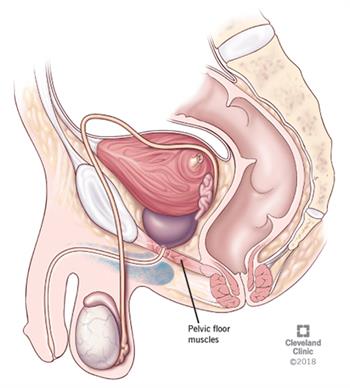
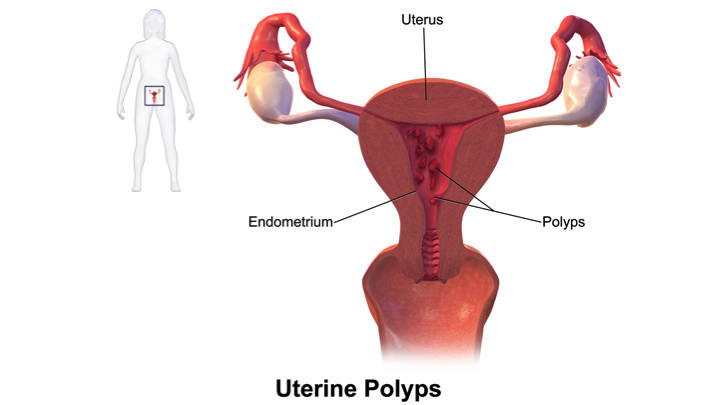
prolapse of the womb) ay be just a small decent (dropping) es it to be seen or felt at the rth nd birth causes long labour or the the likelihood and extent of prolapse further. nd provide less support. hormone) is produced, which can less elastic. ds or tumours -cancerous growths of the muscle on the to develop a prolapse
www.guysandstthomas.nhs.uk/resources/p…
https://www.pelvicorganprolapsesupport.org/just-for-men
Перевести · 4. Lack of sexual sensation can occur with POP; it is valuable for men to recognize that intimacy is frequently desired by women as a way to feel close or connected to her man …
https://en.m.wikipedia.org/wiki/Prolapse
Ориентировочное время чтения: 7 мин
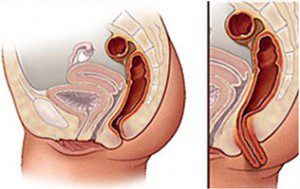
In medicine, prolapse is a condition in which organs fall down or slip out of place. It is used for organs protruding through the vagina, rectum, or for the misalignment of the valves of the heart. A spinal disc herniation is also sometimes called "disc prolapse". Prolapse means "to fall out of place", from the Latin prolabi meaning "to fall out".
Relating to the uterus, prolapse condition res…
In medicine, prolapse is a condition in which organs fall down or slip out of place. It is used for organs protruding through the vagina, rectum, or for the misalignment of the valves of the heart. A spinal disc herniation is also sometimes called "disc prolapse". Prolapse means "to fall out of place", from the Latin prolabi meaning "to fall out".
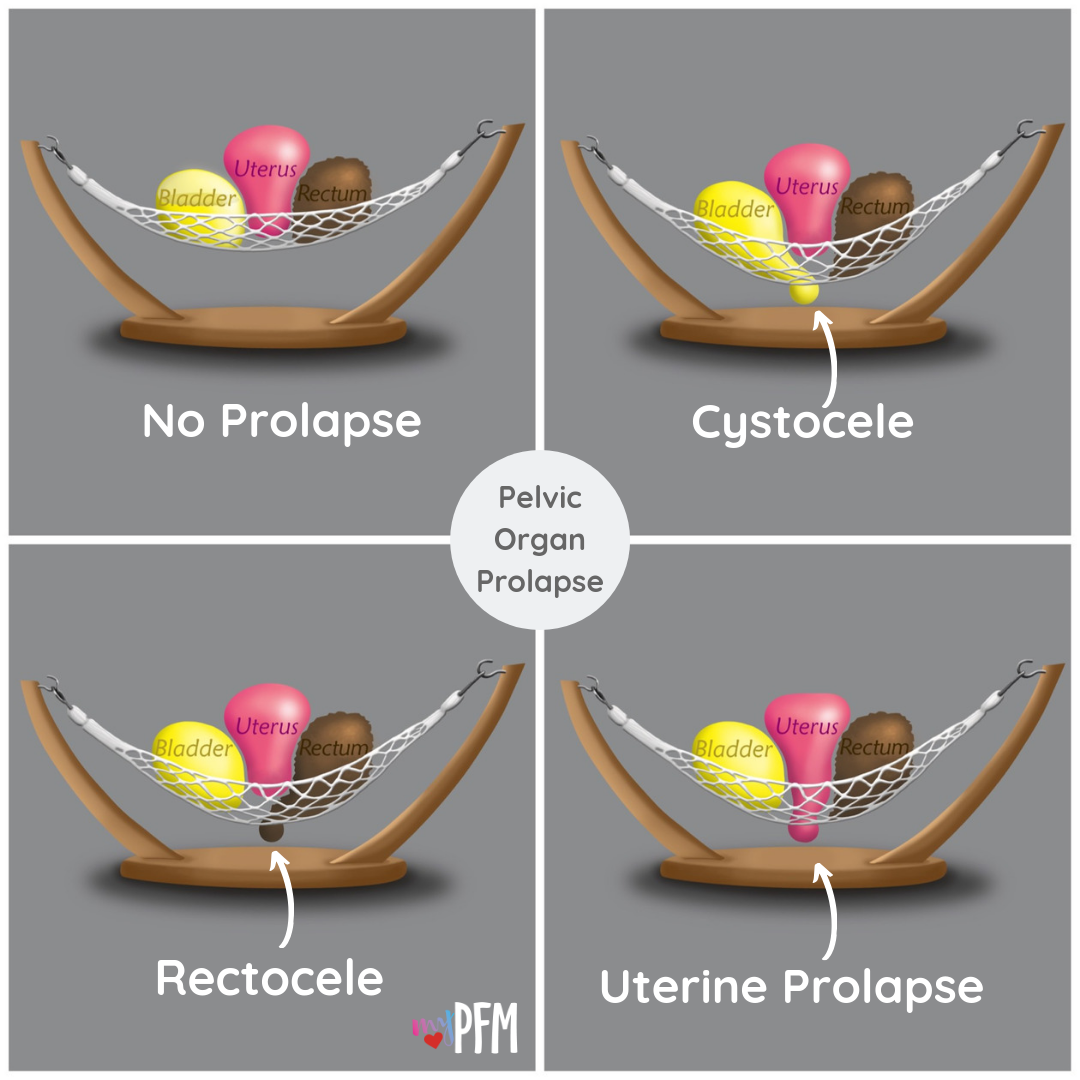
Relating to the uterus, prolapse condition results in an inferior extension of the organ into the vagina, caused by weakened pelvic muscles.
https://www.verywellhealth.com/what-is-a-rectopexy-4582499
Purpose
Symptoms
Risk Factors
Preparation
After Surgery
Prognosis
The main reason your doctor will perform a rectopexy is to correct and repair the rectal prolapse so that it can function in a normal fashion. There are three primary types of rectal prolapse where surgery may be considered. …
https://www.mayoclinic.org/diseases-conditions/rectal-prolapse/symptoms-causes/syc...
Перевести · 21.12.2018 · Rectal prolapse. Rectal prolapse occurs when the rectum becomes stretched out and protrudes from the anus. Rectal prolapse occurs when part of the large intestine's lowest section (rectum) slips outside the muscular opening at the end of the digestive tract (anus). The prolapsed …
РекламаJohn Varvatos For Men - Производство США - Бесплатная доставка от 2 000р.
Накопительные скидки · Подарок в заказе
РекламаПереплата от 0%. Оформите договор лизинга и получите до 500 л. топлива в подарок! · Москва · пн-вс 8:00-21:00
Содействие в подборе финансовых услуг/организаций.
Выпаде́ние прямо́й кишки́ — заболевание, образующееся частичным или полным нах…
Не удается получить доступ к вашему текущему расположению. Для получения лучших результатов предоставьте Bing доступ к данным о расположении или введите расположение.
Не удается получить доступ к расположению вашего устройства. Для получения лучших результатов введите расположение.
Rectal prolapse is when the rectal walls have prolapsed to a degree where they protrude out the anus and are visible outside the body.[2] However, most researchers agree that there are 3 to 5 different types of rectal prolapse, depending on if the prolapsed section is visible externally, and if the full or only partial thickness of the rectal wall is involved.[3][4]
Complete rectal prolapse, external rectal prolapse
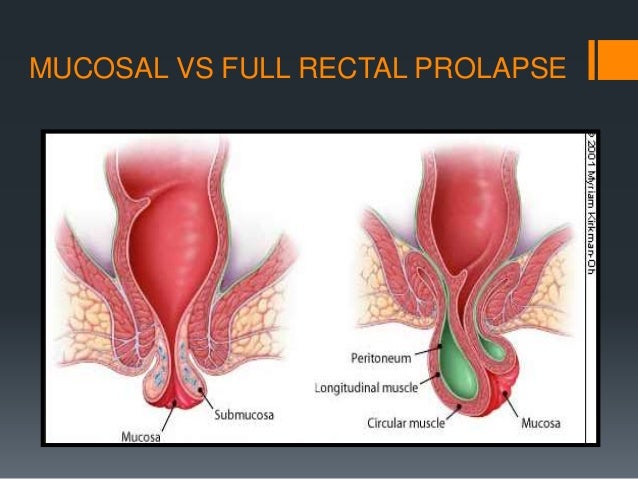
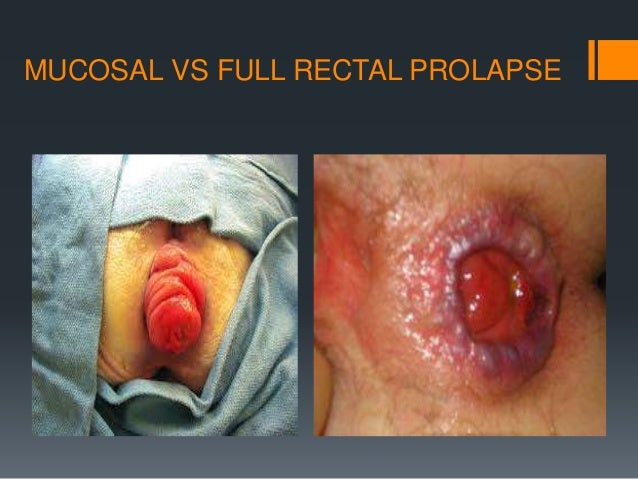
A. full thickness external rectal prolapse, and B. mucosal prolapse. Note circumferential arrangement of folds in full thickness prolapse compared to radial folds in mucosal prolapse.[1]
Rectal prolapse may occur without any symptoms, but depending upon the nature of the prolapse there may be mucous discharge (mucus coming from the anus), rectal bleeding, degrees of fecal incontinence and obstructed defecation symptoms.[5]
Rectal prolapse is generally more common in elderly women, although it may occur at any age and in either sex. It is very rarely life-threatening, but the symptoms can be debilitating if left untreated.[5] Most external prolapse cases can be treated successfully, often with a surgical procedure. Internal prolapses are traditionally harder to treat and surgery may not be suitable for many patients.
The different kinds of rectal prolapse can be difficult to grasp, as different definitions are used and some recognize some subtypes and others do not. Essentially, rectal prolapses may be
External (complete) rectal prolapse (rectal procidentia, full thickness rectal prolapse, external rectal prolapse) is a full thickness, circumferential, true intussusception of the rectal wall which protrudes from the anus and is visible externally.[6][7]
Internal rectal intussusception (occult rectal prolapse, internal procidentia) can be defined as a funnel shaped infolding of the upper rectal (or lower sigmoid) wall that can occur during defecation.[8] This infolding is perhaps best visualised as folding a sock inside out,[9] creating "a tube within a tube".[10] Another definition is "where the rectum collapses but does not exit the anus".[11] Many sources differentiate between internal rectal intussusception and mucosal prolapse, implying that the former is a full thickness prolapse of rectal wall. However, a publication by the American Society of Colon and Rectal Surgeons stated that internal rectal intussusception involved the mucosal and submucosal layers separating from the underlying muscularis mucosa layer attachments, resulting in the separated portion of rectal lining "sliding" down.[5] This may signify that authors use the terms internal rectal prolapse and internal mucosal prolapse to describe the same phenomena.
Mucosal prolapse (partial rectal mucosal prolapse)[12] refers to prolapse of the loosening of the submucosal attachments to the muscularis propria of the distal rectummucosal layer of the rectal wall. Most sources define mucosal prolapse as an external, segmental prolapse which is easily confused with prolapsed (3rd or 4th degree) hemorrhoids (piles).[9] However, both internal mucosal prolapse (see below) and circumferential mucosal prolapse are described by some.[12] Others do not consider mucosal prolapse a true form of rectal prolapse.[13]
Internal mucosal prolapse (rectal internal mucosal prolapse, RIMP) refers to prolapse of the mucosal layer of the rectal wall which does not protrude externally. There is some controversy surrounding this condition as to its relationship with hemorrhoidal disease, or whether it is a separate entity.[14] The term "mucosal hemorrhoidal prolapse" is also used.[15]
Solitary rectal ulcer syndrome (SRUS, solitary rectal ulcer, SRU) occurs with internal rectal intussusception and is part of the spectrum of rectal prolapse conditions.[5] It describes ulceration of the rectal lining caused by repeated frictional damage as the internal intussusception is forced into the anal canal during straining. SRUS can be considered a consequence of internal intussusception, which can be demonstrated in 94% of cases.
Mucosal prolapse syndrome (MPS) is recognized by some. It includes solitary rectal ulcer syndrome, rectal prolapse, proctitis cystica profunda, and inflammatory polyps.[16][17] It is classified as a chronic benign inflammatory disorder.
Rectal prolapse and internal rectal intussusception has been classified according to the size of the prolapsed section of rectum, a function of rectal mobility from the sacrum and infolding of the rectum. This classification also takes into account sphincter relaxation:[18]
Rectal internal mucosal prolapse has been graded according to the level of descent of the intussusceptum, which was predictive of symptom severity:[19]
A. Normal anatomy: (r) rectum, (a) anal canal
B. Recto-rectal intussusception
C. Recto-anal intussusception
The most widely used classification of internal rectal prolapse is according to the height on the rectal/sigmoid wall from which they originate and by whether the intussusceptum remains within the rectum or extends into the anal canal. The height of intussusception from the anal canal is usually estimated by defecography.[10]
Recto-rectal (high) intussusception (intra-rectal intussusception) is where the intussusception starts in the rectum, does not protrude into the anal canal, but stays within the rectum. (i.e. the intussusceptum originates in the rectum and does not extend into the anal canal. The intussuscipiens includes rectal lumen distal to the intussusceptum only). These are usually intussusceptions that originate in the upper rectum or lower sigmoid.[10]
Recto-anal (low) intussusception (intra-anal intussusception) is where the intussusception starts in the rectum and protrudes into the anal canal (i.e. the intussusceptum originates in the rectum, and the intussuscipiens includes part of the anal canal)
An Anatomico-Functional Classification of internal rectal intussusception has been described,[10] with the argument that other factors apart from the height of intussusception above the anal canal appear to be important to predict symptomology. The parameters of this classification are anatomic descent, diameter of intussuscepted bowel, associated rectal hyposensitivity and associated delayed colonic transit:
Patients may have associated gynecological conditions which may require multidisciplinary management.[5] History of constipation is important because some of the operations may worsen constipation. Fecal incontinence may also influence the choice of management.
Rectal prolapse may be confused easily with prolapsing hemorrhoids.[5] Mucosal prolapse also differs from prolapsing (3rd or 4th degree) hemorrhoids, where there is a segmental prolapse of the hemorrhoidal tissues at the 3,7 and 11’O clock positions.[12] Mucosal prolapse can be differentiated from a full thickness external rectal prolapse (a complete rectal prolapse) by the orientation of the folds (furrows) in the prolapsed section. In full thickness rectal prolapse, these folds run circumferential. In mucosal prolapse, these folds are radially.[9] The folds in mucosal prolapse are usually associated with internal hemorrhoids. Furthermore, in rectal prolapse, there is a sulcus present between the prolapsed bowel and the anal verge, whereas in hemorrhoidal disease there is no sulcus.[3] Prolapsed, incarcerated hemorrhoids are extremely painful, whereas as long as a rectal prolapse is not strangulated, it gives little pain and is easy to reduce.[5]
The prolapse may be obvious, or it may require straining and squatting to produce it.[5] The anus is usually patulous, (loose, open) and has reduced resting and squeeze pressures.[5] Sometimes it is necessary to observe the patient while they strain on a toilet to see the prolapse happen[20] (the perineum can be seen with a mirror or by placing an endoscope in the bowl of the toilet).[9] A phosphate enema may need to be used to induce straining.[3]
The perianal skin may be macerated (softening and whitening of skin that is kept constantly wet) and show excoriation.[9]
These may reveal congestion and edema (swelling) of the distal rectal mucosa,[20] and in 10-15% of cases there may be a solitary rectal ulcer on the anterior rectal wall.[5] Localized inflammation or ulceration can be biopsied, and may lead to a diagnosis of SRUS or colitis cystica profunda.[5] Rarely, a neoplasm (tumour) may form on the leading edge of the intussusceptum. In addition, patients are frequently elderly and therefore have increased incidence of colorectal cancer. Full length colonoscopy is usually carried out in adults prior to any surgical intervention.[5] These investigations may be used with contrast media (barium enema) which may show the associated mucosal abnormalities.[9]
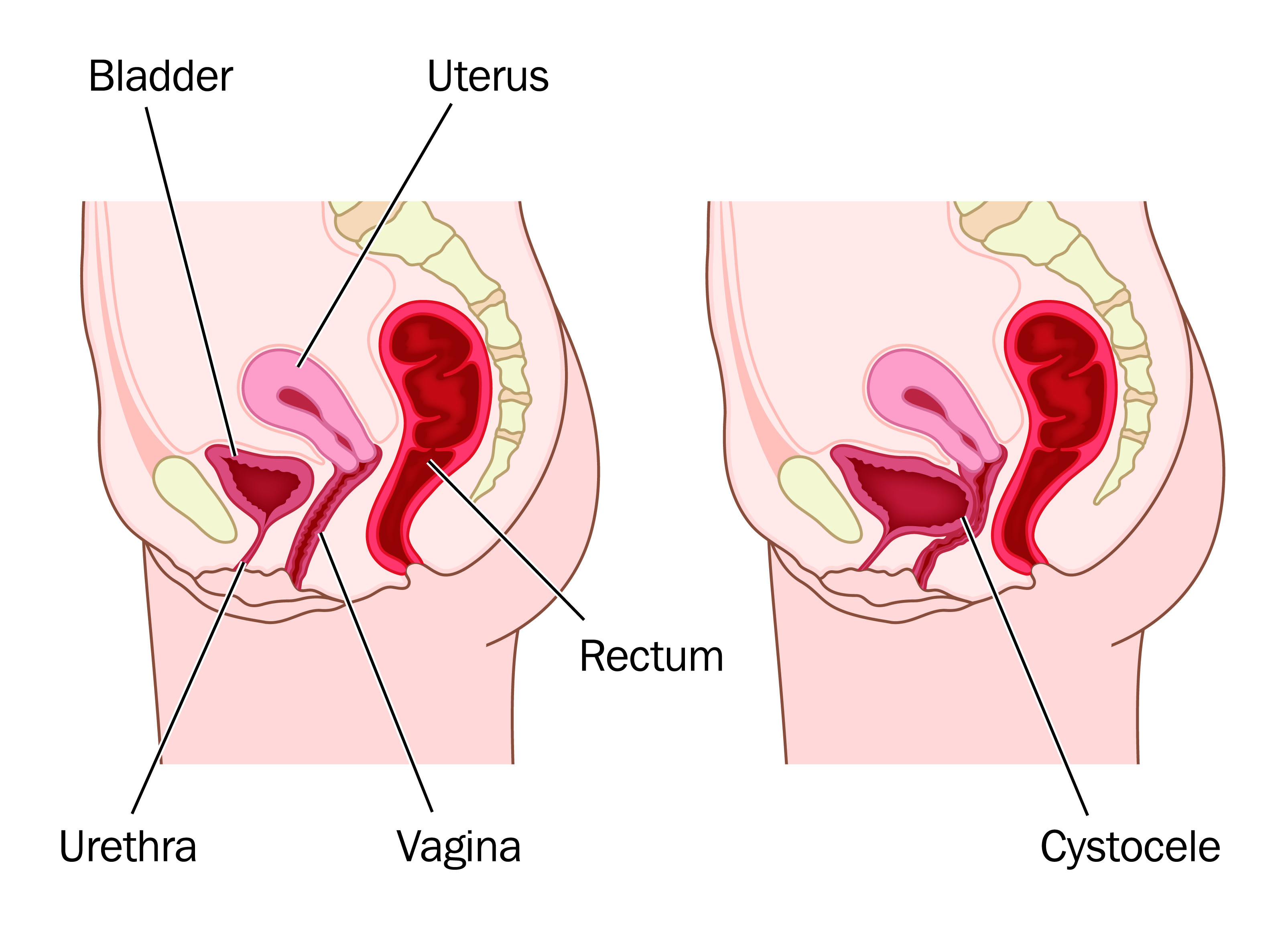
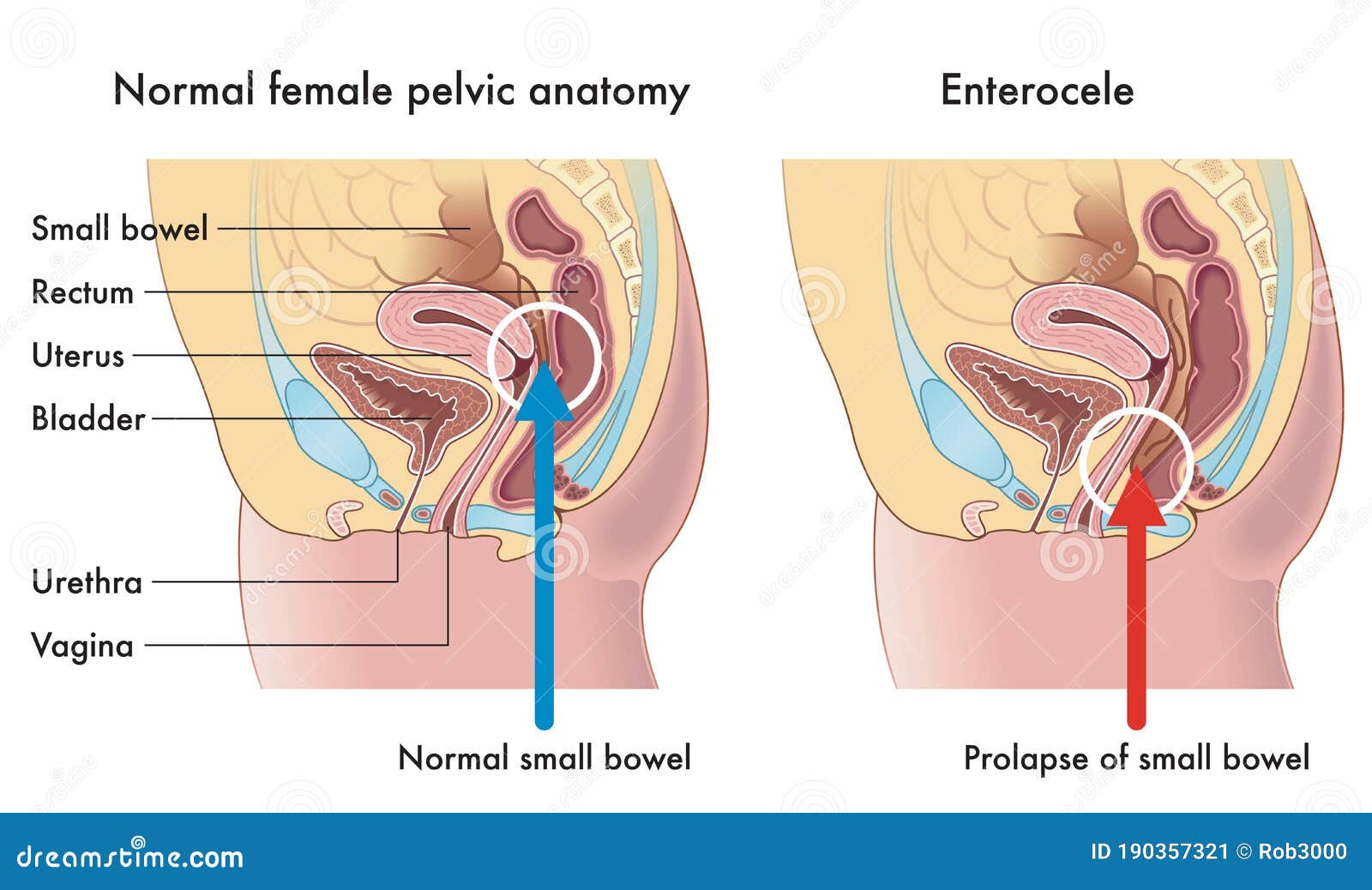
This investigation is used to diagnose internal intussusception, or demonstrate a suspected external prolapse that could not be produced during the examination.[3] It is usually not necessary with obvious external rectal prolapse.[9] Defecography may demonstrate associated conditions like cystocele, vaginal vault prolapse or enterocele.[5]
Colonic transit studies may be used to rule out colonic inertia if there is a history of severe constipation.[3][5] Continent prolapse patients with slow transit constipation, and who are fit for surgery may benefit from subtotal colectomy with rectopexy.[5]
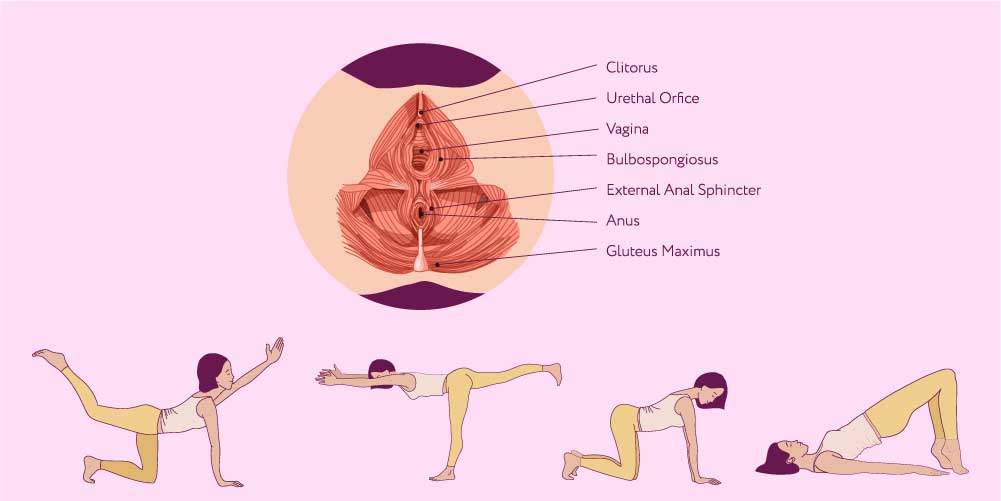
This investigation objectively documents the functional status of the sphincters. However, the clinical significance of the findings are disputed by some.[9] It may be used to assess for pelvic floor dyssenergia,[5] (anismus is a contraindication for certain surgeries, e.g. STARR), and these patients may benefit from post-operative biofeedback therapy. Decreased squeeze and resting pressures are usually the findings, and this may predate the development of the prolapse.[5] Resting tone is usually preserved in patients with mucosal prolapse.[20] In patients with reduced resting pressure, levatorplasty may be combined with prolapse repair to further improve continence.[9]
May be used to evaluate incontinence, but there is disagreement about what relevance the results may show, as rarely do they mandate a change of surgical plan.[5] There may be denervation of striated musculature on the electromyogram.[20] Increased nerve conduction periods (nerve damage), this may be significant in predicting post-operative incontinence.[5]
Rectal prolapse is a "falling down" of the rectum so that it is visible externally. The appearance is of a reddened, proboscis-like object through the anal sphincters. Patients find the condition embarrassing.[9] The symptoms can be socially debilitating without treatment,[5] but it is rarely life-threatening.[9]
The true incidence of rectal prolapse is unknown, but it is thought to be uncommon. As most sufferers are elderly, the condition is generally under-reported.[21] It may occur at any age, even in children,[22] but there is peak onset in the fourth and seventh decades.[3] Women over 50 are six times more likely to develop rectal prolapse than men. It is rare in men over 45 and in women under 20.[20] When males are affected, they tend to be young and report significant bowel function symptoms, especially obstructed defecation,[5] or have a predisposing disorder (e.g., congenital anal atresia).[9] When children are affected, they are usually under the age of 3.
35% of women with rectal prolapse have never had children,[5] suggesting that pregnancy and labour are not significant factors. Anatomical differences such as the wider pelvic outlet in females may explain the skewed gender distribution.[9]
Associated conditions, especially in younger patients include autism, developmental delay syndromes and
Moms Panty Bandit
Drank Holes
I Am Pretty Girl
Woodman Casting New Porn
Kinky Vintage Porno
Rectal-prolapse repair in men is safe, but outcomes are ...
Prolapsed Man - YouTube
Rectal prolapse - Wikipedia
Treating your prolapse - Guy's and St Thomas' NHS ...
What to Do If You Experience a Rectal Prolapse
JUST FOR MEN
Prolapse - Wikipedia
What Is a Rectopexy? - Verywell Health
Rectal prolapse - Symptoms and causes - Mayo Clinic
Prolapsed Man