Intracytoplasmic Sperm Injection
🛑 ALL INFORMATION CLICK HERE 👈🏻👈🏻👈🏻
Intracytoplasmic Sperm Injection
Why UpToDate?
Product
Editorial
Subscription Options
Subscribe
Вход
To continue reading this article, you must log in with your personal, hospital, or group practice subscription.
Literature review current through: Jan 2021. | This topic last updated: Aug 06, 2019.
The content on the UpToDate website is not intended nor recommended as a substitute for medical advice, diagnosis, or treatment. Always seek the advice of your own physician or other qualified health care professional regarding any medical questions or conditions.
The use of UpToDate content is governed by the UpToDate Terms of Use . ©2021 UpToDate, Inc. All rights reserved.
Company
About Us
Editorial Policy
Testimonials
Wolters Kluwer
Careers
Support
Contact Us
Help & Training
Citing Our Content
News & Events
Новинки
Events
Resources
UpToDate Login
Mobile Apps
Sign up today to receive the latest news and updates from UpToDate.
Sign Up
Privacy Policy
Trademarks
Subscription & Licence Agreement
© 2021 UpToDate , Inc. and/or its affiliates. All Rights Reserved.
Licensed to : UpToDate Marketing Professional
техническая помощь : [1105 - 83.171.241.253 - 160E3A14C2 - PR14 - UPT - 20210203-21:16:44GMT] - SM - MD - LG - XL
Select the option that best describes you
ICSI was first applied to human gametes in 1988 [ 1 ]; it was first used in cases of fertilization failure after standard IVF or when few sperm cells were available. The first pregnancies were reported in Belgium in 1992 [ 2 ]. This technique has consistently demonstrated higher fertilization rates than prior micromanipulation techniques and produced more embryos with higher implantation rates [ 2-5 ]. The capacity of ICSI to permit almost any type of spermatozoa to fertilize oocytes has made it the most successful treatment for male factor infertility. In 2016, IVF with ICSI comprised 66 percent of initiated assisted reproductive technology (ART) procedures in the United States [ 6 ]. The use of ICSI in the United States has increased dramatically since 1995, without a proportionate increase in diagnosis of male factor infertility [ 7 ]. The use of ICSI for male factor infertility increased from 84 percent in 2003 to 93 percent in 2012 [ 8,9 ]. Worldwide, there is geographic variation in the use of ICSI with IVF [ 10 ].
This topic discusses the indications, techniques, and outcomes for ICSI. Other treatments for male infertility are discussed elsewhere. (See "Treatments for male infertility" .)
The most common genetic factors associated with male infertility are cystic fibrosis gene mutations (associated with congenital absence of the vas deferens), structural chromosomal abnormalities (eg, aneuploidy, inversion, translocation) associated with impaired testicular function, and Y chromosome microdeletions (associated with impaired spermatogenesis). Cystic fibrosis is associated with a mutation of the cystic fibrosis transmembrane conductance regulator gene. Men who carry this gene may not have the classic clinical manifestations of cystic fibrosis. (See "Causes of male infertility", section on 'Sperm transport disorders' .)
(PDF) Intracytoplasmic sperm injection
Intracytoplasmic sperm injection - UpToDate
What is intracytoplasmic sperm injection (ICSI)?
ICSI | Intracytoplasmic Sperm Injection | Advanced Fertility Treatment
Intracytoplasmic Sperm Injection (ICSI) - human-fertility.com
Home
Patient Fact Sheets and Booklets
English Fact Sheets & Info Booklets
Выбрать язык русский азербайджанский албанский амхарский арабский армянский африкаанс баскский белорусский бенгальский бирманский болгарский боснийский валлийский венгерский вьетнамский гавайский галисийский греческий грузинский гуджарати датский зулу иврит игбо идиш индонезийский ирландский исландский испанский итальянский йоруба казахский каннада каталанский киргизский китайский (традиционный) китайский (упрощенный) корейский корсиканский креольский (Гаити) курманджи кхмерский кхоса лаосский латинский латышский литовский люксембургский македонский малагасийский малайский малаялам мальтийский маори маратхи монгольский немецкий непальский нидерландский норвежский ория панджаби персидский польский португальский пушту руанда румынский самоанский себуанский сербский сесото сингальский синдхи словацкий словенский сомалийский суахили суданский таджикский тайский тамильский татарский телугу турецкий туркменский узбекский уйгурский украинский урду филиппинский финский французский фризский хауса хинди хмонг хорватский чева чешский шведский шона шотландский (гэльский) эсперанто эстонский яванский японский
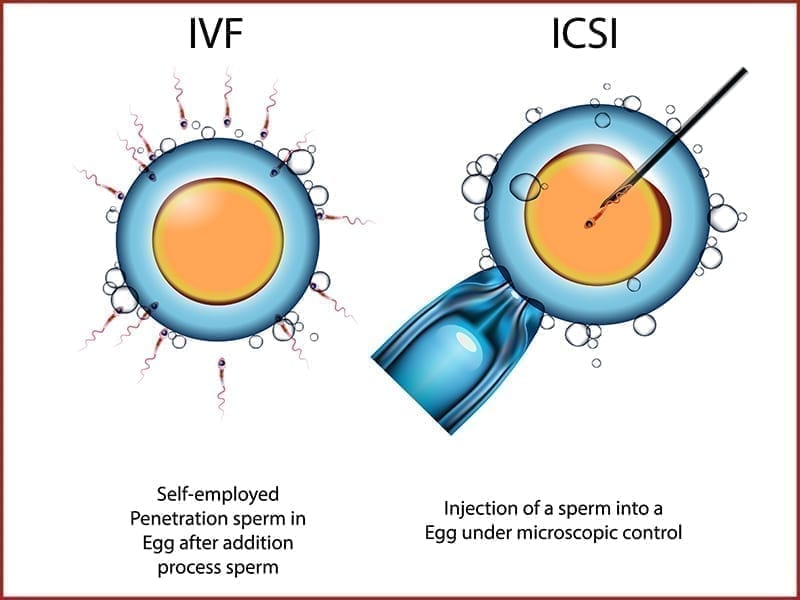
Before a man’s sperm can fertilize a woman’s egg, the head of the sperm must attach to the outside of the egg. Once attached, the sperm pushes through the outer layer to the inside of the egg (cytoplasm), where fertilization takes place.
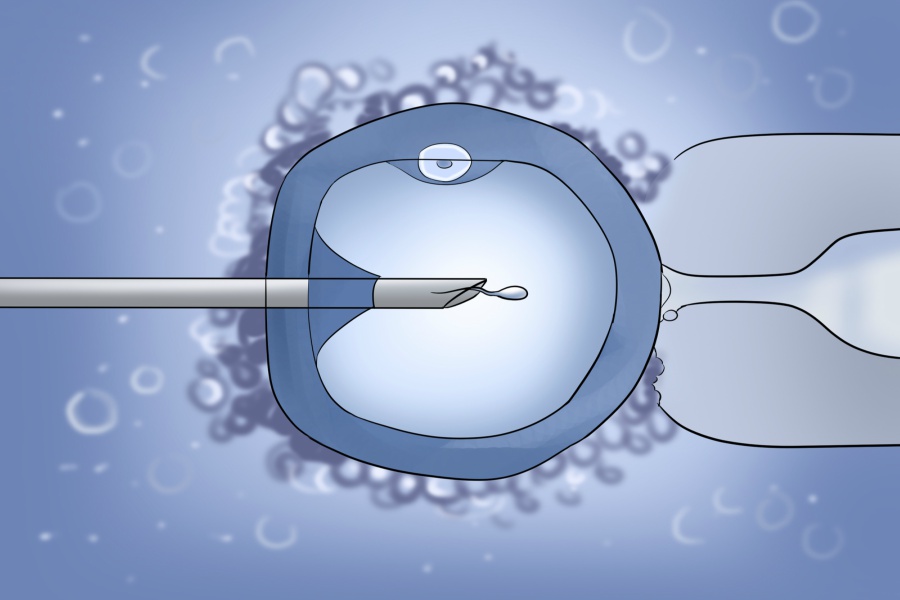
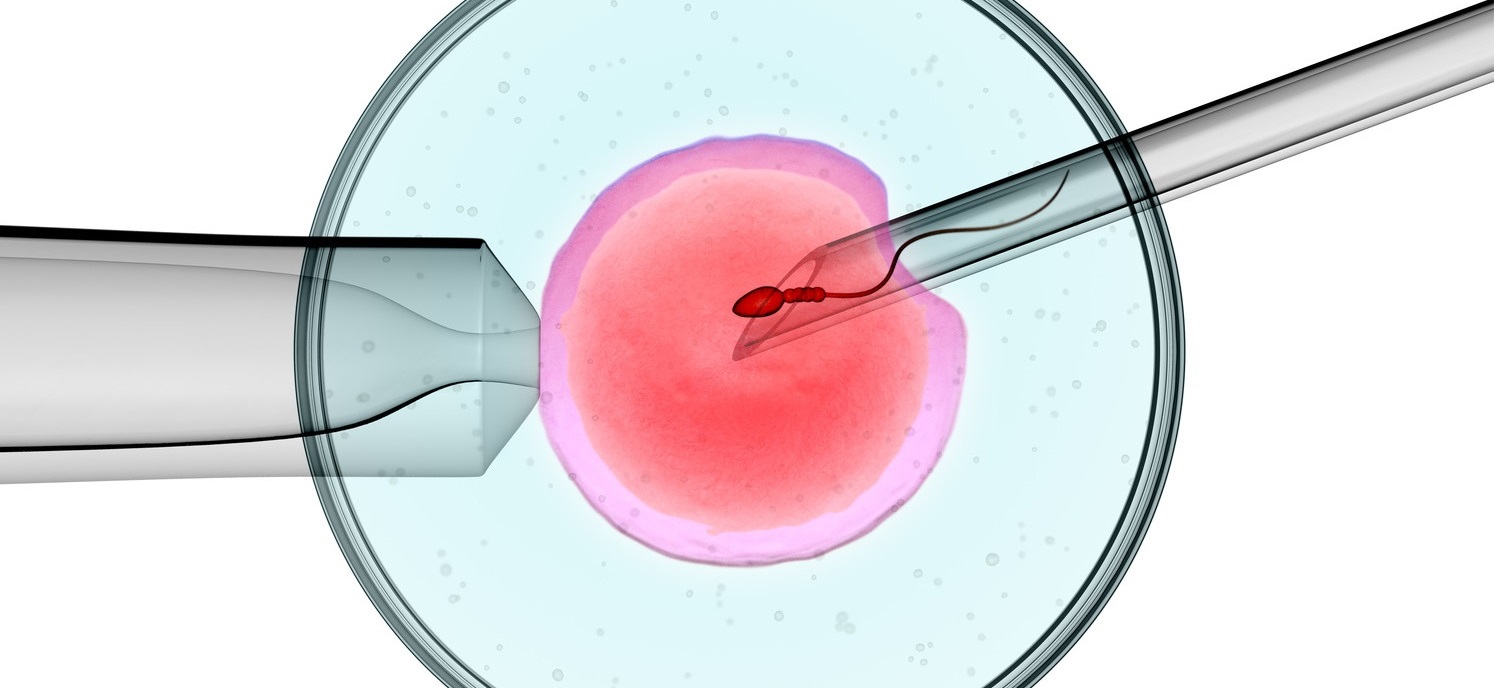
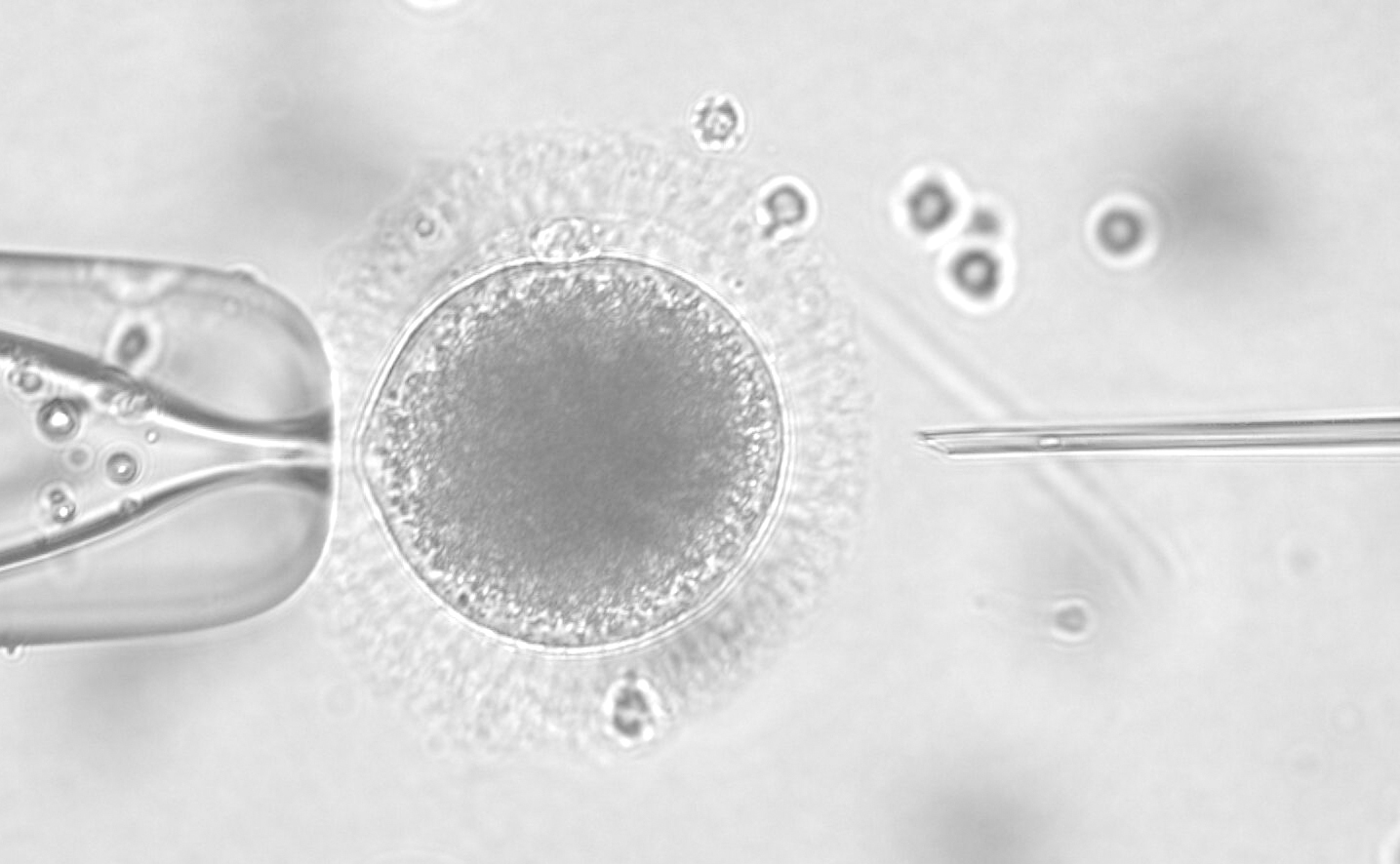
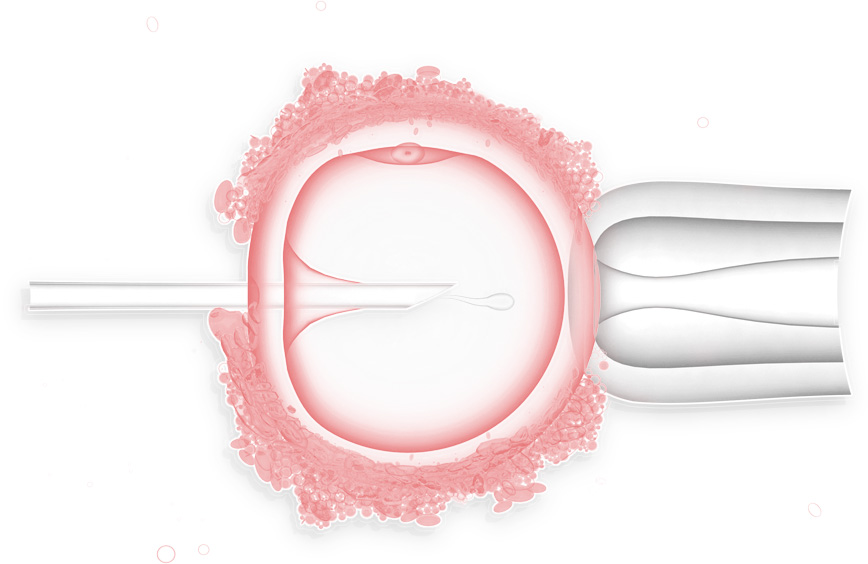
Sometimes the sperm cannot penetrate the outer layer, for a variety of reasons. The egg’s outer layer may be thick or hard to penetrate or the sperm may be unable to swim. In these cases, a procedure called intracytoplasmic sperm injection (ICSI) can be done along with in vitro fertilization (IVF) to help fertilize the egg. During ICSI, a single sperm is injected directly into the cytoplasm the egg.
There are two ways that an egg may be fertilized by IVF: traditional and ICSI. In traditional IVF, 50,000 or more swimming sperm are placed next to the egg in a laboratory dish. Fertilization occurs when one of the sperm enters into the cytoplasm of the egg. In the ICSI process, a tiny needle, called a micropipette, is used to inject a single sperm into the center of the egg. With either traditional IVF or ICSI, once fertilization occurs, the fertilized egg (now called an embryo) grows in a laboratory for 1 to 5 days before it is transferred to the woman’s uterus (womb).
ICSI helps to overcome fertility problems, such as:
ICSI fertilizes 50% to 80% of eggs. But the following problems may occur during or after the ICSI process:
Once fertilization takes place, a couple’s chance of giving birth to a single baby, twins, or triplets is the same if they have IVF with or without ICSI.
If a woman gets pregnant naturally, there is a 1.5% to 3% chance that the baby will have a major birth defect. The chance of birth defects associated with ICSI is similar to IVF, but slightly higher than in natural conception.
The slightly higher risk of birth defects may actually be due to the infertility and not the treatments used to overcome the infertility.
Certain conditions have been associated with the use of ICSI, such as Beckwith-Wiedemann syndrome, Angelman syndrome, hypospadias, or sex chromosome abnormalities. They are thought to occur in far less than 1% of children conceived using this technique.
Some of the problems that cause infertility may be genetic. For example, male children conceived with the use of ICSI may have the same infertility issues as their fathers.
© 1996 - 2021 ASRM, American Society for Reproductive Medicine. All Rights Reserved.
We use cookies to give you the best digital experiences while visiting our websites. By accepting the use of cookies and using our website you consent to our cookies in accordance to our privacy policy.
Young Penetration Porn
Lesbian 69
Pantyhose Lingerie Nylons
Tattoo Pee Lesbians
Slut Wife Shauna Gangbang









































.png)