Clairet Prolapse
🔞 ALL INFORMATION CLICK HERE 👈🏻👈🏻👈🏻
Clairet Prolapse
star
star
star
star
star
format_list_bulleted Contents
add
remove
Summary
Umbilical cord prolapse occurs when the cord descends through the cervix and is alongside or below the presenting part of the fetus.
It is an obstetric emergency, with a fetal mortality rate of 91 per 1000.
The diagnosis should be suspected in any patient with a non-reassuring fetal heart trace and absent membranes.
The first step is to call for help when the diagnosis is made.
Manage by manually elevating the presenting part, and deliver via the quickest mode (usually Caesarean section).
MRP, 2020
Cardiology Advisor, 2020
360Dx, 2017
staff reporter,
360Dx, 2018
Privacy policy
Do not sell my personal information
Google Analytics settings
I consent to the use of Google Analytics and related cookies across the TrendMD network (widget, website, blog). Learn more
[caption id="attachment_14008" align="aligncenter" width="312"] Fig 1 - A footling breech and umbilical cord prolapse.[/caption]
[caption id="attachment_14003" align="aligncenter" width="531"] Fig 2 - The knee-chest position, used in the management of cord prolapse.[/caption]
reply Go back
edit Edit this article
© TeachMe Series 2021 | Registered in England & Wales
reply Go back
edit Edit this article
Original Author(s): Leena Khan Last updated: 22nd December 2017
Revisions: 21
Original Author(s): Leena Khan Last updated: 22nd December 2017
Revisions: 21
Umbilical cord prolapse is where the umbilical cord descends through the cervix, with (or before) the presenting part of the fetus. It affects 0.1 – 0.6% of births.
Cord prolapse occurs in the presence of ruptured membranes, and is either occult or overt:
Although the incidence is relatively low, the mortality rate for such babies is high (~91 per 1000). This is largely because cord prolapse occurs more frequently in preterm babies, who are often breech, and who may also have other congenital defects .
In this article, we shall look at the risk factors, clinical features and management of cord prolapse.
Umbilical cord prolapse is where the umbilical cord descends through the cervix, with (or before) the presenting part of the fetus. Subsequently, f etal hypoxia occurs via two main mechanisms:
The main risk factors for cord prolapse include:
Fig 1 – A footling breech and umbilical cord prolapse.
Cord prolapse should always be considered in the presence of a non-reassuring fetal heart rate pattern and absent membranes. It can be confirmed by external inspection or on digital vaginal examination. This is one of the reasons that vaginal assessment, after abdominal examination, encompasses a full assessment in the presence of a non-reassuring fetal heart rate pattern.
The fetal heart rate patterns can vary from subtle changes, such as decelerations with some of the contractions, to more obvious signs of fetal distress, such as a fetal bradycardia . The latter is strongly associated with cord prolapse; relating to the mechanism of occlusion of the cord by the presenting part.
An alternative diagnosis may be considered in the presence of bleeding per vagina or heavily blood-stained liquor with ruptured membranes. This would suggest placental abruption (the placenta starts to separate from the uterine wall) or vasa praevia (fetal vessels running in the fetal membranes adjacent to the internal os of the cervix).
Firstly, call for help – umbilical cord prolapse is an obstetric emergency . It should be managed as follows:
Fig 2 – The knee-chest position, used in the management of cord prolapse.
Which statement correctly describes an overt cord prolapse?
Try again to score 100%. Use the information in this article to help you with the answers.
Umbilical cord prolapse is where the umbilical cord descends through the cervix, with (or before) the presenting part of the fetus. It affects 0.1 - 0.6% of births.
Cord prolapse occurs in the presence of ruptured membranes, and is either occult or overt:
Although the incidence is relatively low, the mortality rate for such babies is high (~91 per 1000). This is largely because cord prolapse occurs more frequently in preterm babies, who are often breech, and who may also have other congenital defects .
In this article, we shall look at the risk factors, clinical features and management of cord prolapse.
Umbilical cord prolapse is where the umbilical cord descends through the cervix, with (or before) the presenting part of the fetus. Subsequently, f etal hypoxia occurs via two main mechanisms:
The main risk factors for cord prolapse include:
Cord prolapse should always be considered in the presence of a non-reassuring fetal heart rate pattern and absent membranes. It can be confirmed by external inspection or on digital vaginal examination. This is one of the reasons that vaginal assessment, after abdominal examination, encompasses a full assessment in the presence of a non-reassuring fetal heart rate pattern.
The fetal heart rate patterns can vary from subtle changes, such as decelerations with some of the contractions, to more obvious signs of fetal distress, such as a fetal bradycardia . The latter is strongly associated with cord prolapse; relating to the mechanism of occlusion of the cord by the presenting part.
An alternative diagnosis may be considered in the presence of bleeding per vagina or heavily blood-stained liquor with ruptured membranes. This would suggest placental abruption (the placenta starts to separate from the uterine wall) or vasa praevia (fetal vessels running in the fetal membranes adjacent to the internal os of the cervix).
Firstly, call for help - umbilical cord prolapse is an obstetric emergency . It should be managed as follows:
Found an error? Is our article missing some key information? Make the changes yourself here!
Once you've finished editing, click 'Submit for Review', and your changes will be reviewed by our team before publishing on the site.
The medical information on this site is provided as an information resource only, and is not to be used or relied on for any diagnostic or treatment purposes. This information is intended for medical education, and does not create any doctor-patient relationship, and should not be used as a substitute for professional diagnosis and treatment.
By visiting this site you agree to the foregoing terms and conditions. If you do not agree to the foregoing terms and conditions, you should not enter this site.
Found an error? Is our article missing some key information? Make the changes yourself here!
Once you've finished editing, click 'Submit for Review', and your changes will be reviewed by our team before publishing on the site.
Prolapsed Uterus After Childbirth: What You... | Crystal Run Healthcare
Umbilical Cord Prolapse - Risk Factors - Management - TeachMeObGyn
Rectal Prolapse : Symptoms, Treatment, and More
Prolapse - Home | Facebook
Uterine prolapse - Wikipedia
Medically reviewed by Judith Marcin, M.D. — Written by James Roland — Updated on May 1, 2017
Medically reviewed by Judith Marcin, M.D. — Written by James Roland — Updated on May 1, 2017
© 2005-2021 Healthline Media a Red Ventures Company. All rights reserved. Our website services, content, and products are for informational purposes only. Healthline Media does not provide medical advice, diagnosis, or treatment. See additional information .
© 2005-2021 Healthline Media a Red Ventures Company. All rights reserved. Our website services, content, and products are for informational purposes only. Healthline Media does not provide medical advice, diagnosis, or treatment. See additional information .
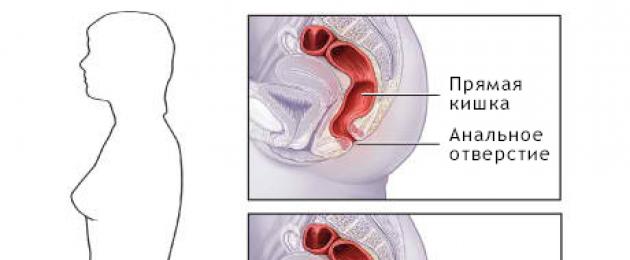
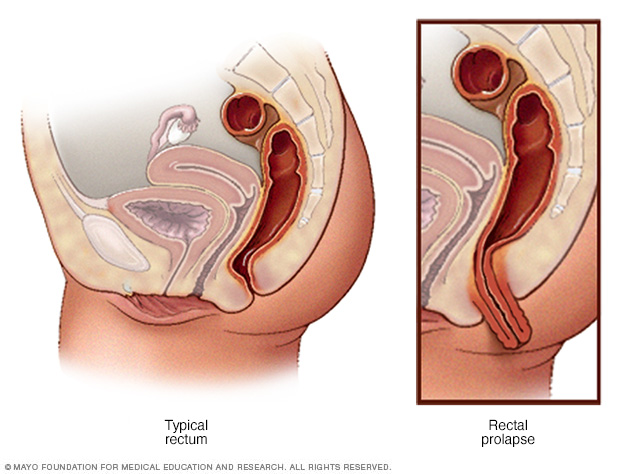
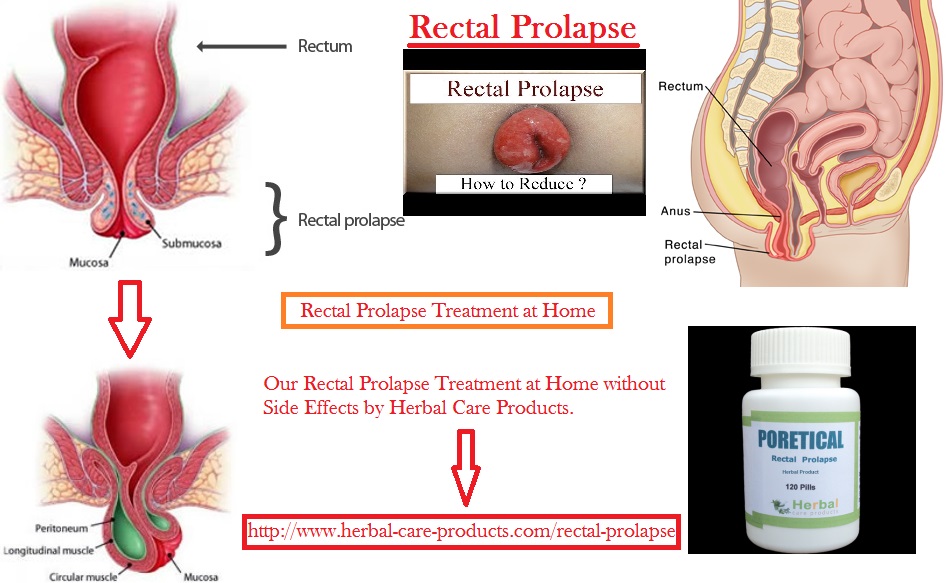
Rectal prolapse is a medical condition in which the rectum starts to push through the anus. The rectum is that last part of your large intestine, and the anus is the opening through which stool exits your body.
Rectal prolapse affects about 2.5 people out of 100,000 . Women over 50 are six times more likely than men to have this condition. It’s often suspected when the problem is actually a serious case of hemorrhoids.
Rectal prolapse can range from mild to severe. Mild cases can often be treated without surgery. Severe cases may require surgery.
The symptoms of rectal prolapse tend to come on slowly. The first symptom you’ll notice is the feeling that there is a bulge at your anus. It may seem as though you are sitting on a ball.
With a mirror, you may be able to see a reddish-colored bulge peeking through or actually extending out of your anus. Sometimes during a bowel movement, a small part of the rectum will emerge, but may retreat on its own or be easily pushed back into place.
Normal physical activity, such as walking, sitting, and exercising, may also cause part of the rectum to push through your anus. At first, it can be returned to its proper location by hand.
If rectal prolapse worsens, there could be bleeding from the inner lining of the rectum. In cases of partial or complete prolapse, you may have trouble controlling liquid or solid bowel movement and gas from your rectum.
Up to half of the people with rectal prolapse experience constipation, while others may have episodes of constipation and incontinence.
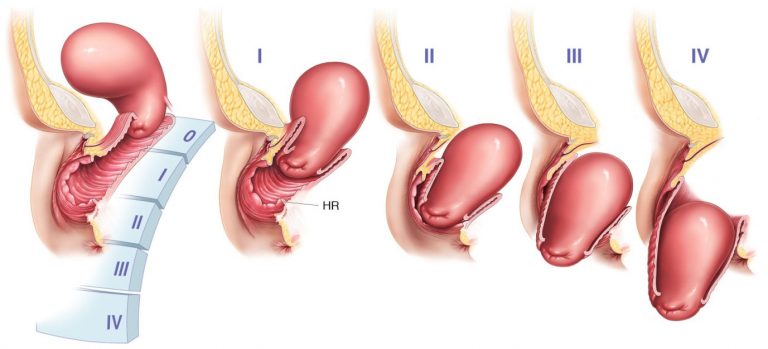
There are three types of rectal prolapse. The type is identified by the movement of the rectum:
Rectal prolapse can be caused by several medical conditions. They include:
If nerves that control the rectal and anal muscles are damaged, rectal prolapse can develop. These nerves can sometimes be damaged from:
This is the muscle that allows stool to pass from your rectum. Common reasons for this muscle to weaken are pregnancy and childbirth, or increased age.
The strain of chronic bowel movement problems can make your rectum more likely to move down from its location. Strain while having bowel movements, if done often over a period of years, can also cause rectal prolapse.
While not directly linked to rectal prolapse, some conditions may increase your risk for it, including:
Women over the age of 50 are also at an increased risk of rectal prolapse.
Rectal prolapse and hemorrhoids can both be uncomfortable and very painful conditions. Rectal prolapse may initially feel like a bad case of hemorrhoids, and sometimes hemorrhoids on your anus may look as though your rectum is emerging.
Rectal prolapse involves movement of the rectum itself. Hemorrhoids are actually swollen blood vessels in the walls of your rectum or anus. Hemorrhoids, though quite common in their smaller, milder form, can become painful and itchy. They can leave red blood on tissue when you wipe. Rectal prolapse can also cause bleeding sometimes.
If you suspect you have hemorrhoids or rectal prolapse, see your doctor. They can diagnose your condition and start the appropriate treatment.
Your doctor will have you describe your symptoms and ask about your medical history. They should also do a complete physical examination. During your exam, your doctor may ask you to squat and strain as though you were having a bowel movement. Your doctor will observe your rectum and may placed a gloved finger in your anus to check the health or strength of the anal sphincter and the rectum itself.
You may also be directed to have a colonoscopy to check for any polyps.
Rectal prolapse won’t get better on its own. The degree of prolapse will increase over time. This process can take months or years, so there isn’t always a rush to make a decision.
If you’ve been diagnosed with rectal prolapse, you may choose to delay treatment if your symptoms are mild enough and your quality of life isn’t significantly hampered.
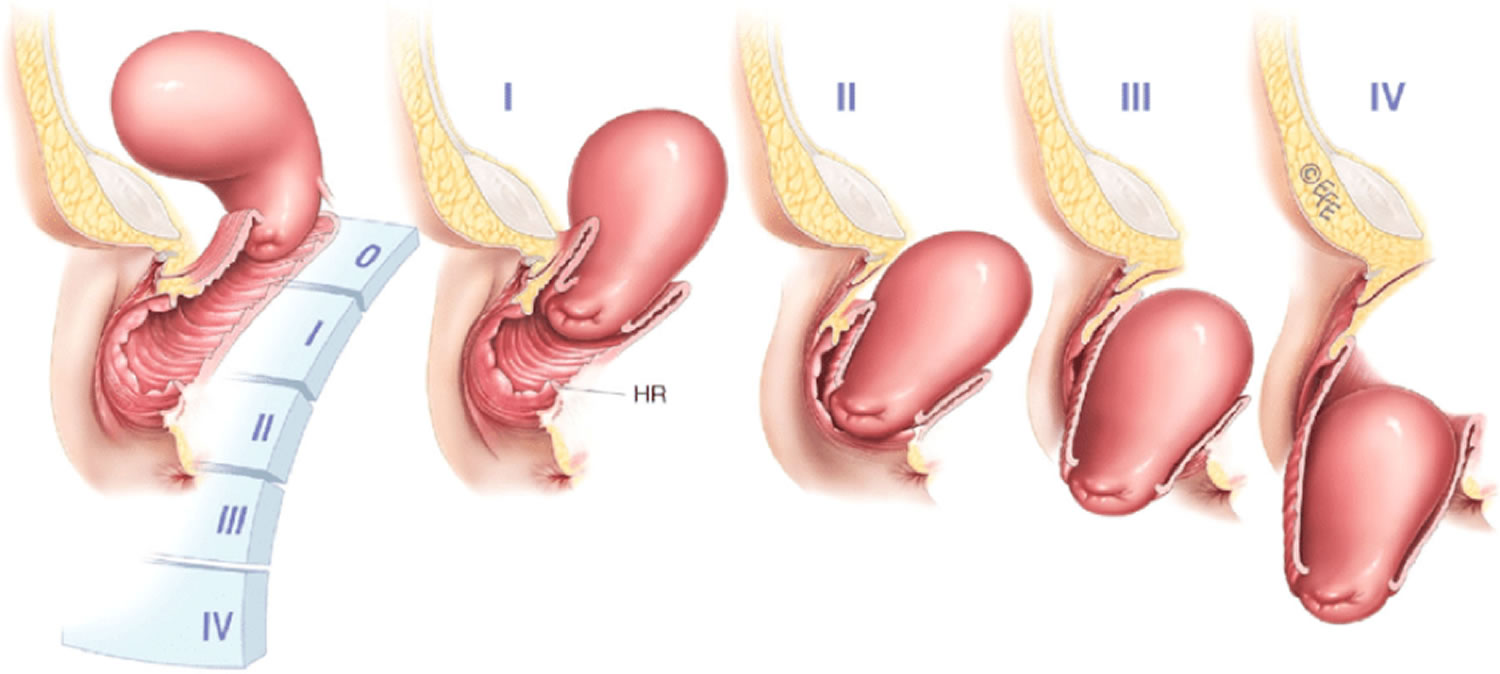
Surgery is the only way to effectively treat rectal prolapse and relieve symptoms. The surgeon can do the surgery through the abdomen or through the area around the anus.
Surgery through the abdomen is performed to pull the rectum back up and into its proper position. It can be done with a large incision and open surgery, or it can be done laparoscopically, using a few incisions and specially designed smaller surgical tools.
Surgery from the region around the anus involves pulling part of the rectum out and surgically removing it. The rectum is then placed back inside and attached to the large intestine. This approach is usually performed in people who aren’t good candidates for surgery through their abdomen.
Discuss your options with your doctor. If they recommend one type of surgery, you should feel comfortable asking why it’s recommended.
The outlook is generally positive for someone undergoing rectal prolapse surgery. You’ll be on a diet of liquids and soft foods for a while, and you’ll need to take a stool softener at first. This is to prevent constipation or straining during a bowel movement.
The amount of time spent in the hospital after surgery depends on your health and the type of surgery you had. A full recovery can be expected in about six weeks.
Rectal prolapse can be uncomfortable and painful, but it’s treatable. The sooner you see a doctor about your symptoms, the easier the surgery and recovery.
Preventing rectal prolapse isn’t always possible. You can reduce your risk if you maintain good intestinal health. To help avoid constipation, in particular:
Last medically reviewed on May 1, 2017





















 f_auto" width="550" alt="Clairet Prolapse" title="Clairet Prolapse">w_1920/v1560143800/gu0t0urovobjh05qzvgo.jpg" width="550" alt="Clairet Prolapse" title="Clairet Prolapse">
f_auto" width="550" alt="Clairet Prolapse" title="Clairet Prolapse">w_1920/v1560143800/gu0t0urovobjh05qzvgo.jpg" width="550" alt="Clairet Prolapse" title="Clairet Prolapse">